What Is Lymphedema?
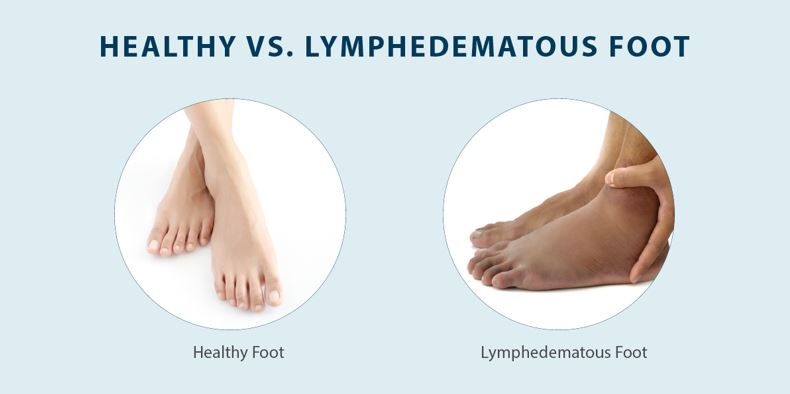
Lymphedema is a medical condition that causes swelling as a result of built-up fluid in your tissues. In a healthy body, fluid flows through your lymph vessels and nodes before returning to your bloodstream, but a blockage or damage can cause fluid to build up in the area. This buildup of fluid can accumulate in the surrounding tissue and cause swelling, which is the primary symptom of lymphedema. While lymphedema mostly affects the arms and legs, lymphedema in feet and other areas is also a possibility.
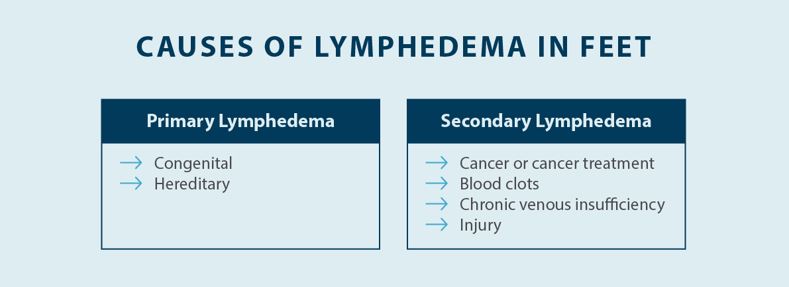
There are two distinct types of lymphedema — primary lymphedema and secondary lymphedema. Lymphedema that occurs as a result of genetics, known as hereditary lymphedema, or lymphedema that is congenital and present at birth, is considered primary lymphedema. However, primary lymphedema symptoms can take several years or even decades to present, and there are different names for it depending on the onset of symptoms. The more common type of lymphedema is secondary lymphedema, which can be caused by cancer and cancer treatment, an acute injury, disease, or another factor that’s unrelated to genetics.
The causes of primary lymphedema can be challenging to identify. Primary lymphedema is thought to be linked to a several gene mutations, such as a genetic mutation involving the FOXC2 gene, leading to lymphedema that typically develops during or after puberty, which is also known as lymphedema praecox.1 In some cases, people with primary lymphedema don’t experience swelling and other symptoms until they’re over the age of 35, which is known as lymphedema tarda.2 While there’s no exact known cause of primary lymphedema, research suggests that genetics may play a role. However, classification of primary lymphedema moving away from solely classifying primary lymphedema based on the age of onset to a classification system that involves phenotyping, called St. George’s Classification Algorithm of Primary Lymphatic Anomalies.3
Secondary lymphedema has many potential causes. Secondary lymphedema can be caused by cancer, cancer surgery, or radiation therapy. Cancer that affects your lymphatic system or leads to lymph node removal can cause a disruption in your lymphatic system, leading to swelling in the affected area. In patients who haven’t had cancer, lymphedema can be caused by chronic venous disease, acute injuries to the lymphatic system, infections, and certain disease or medications. There are also several risk factors for lymphedema, including obesity and prolonged sitting or standing.
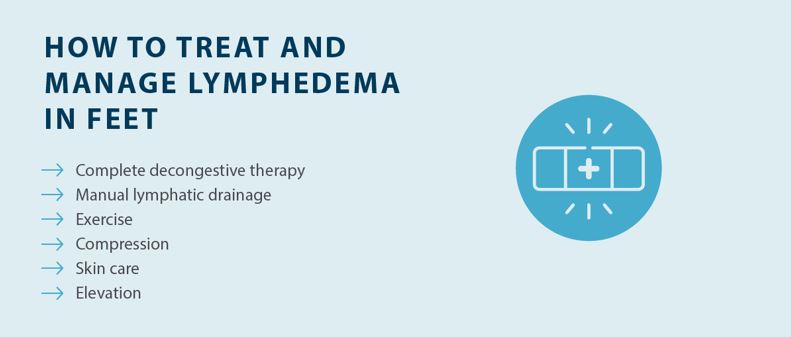
Getting a diagnosis is an essential part of treating lymphedema because there are so many different types and potential causes. Reducing swelling and reducing the progression of symptoms is a primary focus in managing lymphedema. If you have symptoms of lymphedema in your feet or any other area of your body, it’s recommended to schedule an appointment with your doctor.