What Is Complete Decongestive Therapy?


Complete decongestive therapy (CDT) is a treatment for lymphedema, edema, and similar conditions where swelling is present. Unlike other types of treatment for lymphedema, complete decongestive therapy doesn’t refer to a single treatment method. Instead, CDT combines several different treatment methods to help stimulate the lymphatic system and relieve the pain, swelling, and other symptoms that may be present with lymphedema.
Because lymphedema is a lifelong condition, the goal of CDT is to provide relief from the symptoms that make lymphedema difficult and prevent its progression. CDT can help people who have a loss of range of motion, pain, swelling, skin changes and/or a lack of mobility as a result of lymphedema.
While complete decongestive therapy for lymphedema can be a good treatment option, you should always talk to a doctor or specialist before starting any treatment. If you’re considering complete decongestive therapy for lipedema or lymphedema treatment, read below to learn more about how CDT is performed.
What Does Complete Decongestive Therapy Treat?
Complete decongestive therapy is used to treat edema, lipedema, lymphedema, and similar conditions. While there are several conditions that CDT can treat, it’s most often used to treat the various forms of edema. Complete decongestive therapy can be used to treat both congenital and hereditary lymphedema.
Lymphedema is swelling that occurs when excess fluid builds up in your body’s tissues. This buildup can result from a blockage or malfunction in the lymphatic system, or it can be inherited or present at birth. When there is an interruption in the flow of fluid, localized pain and swelling can occur, and can be the result of damage to the lymph nodes, lymph vessels, and other parts of the lymphatic system.
While complete decongestive therapy is often used on lymphedema patients, it can also be used to treat other conditions that cause localized swelling. Some conditions that complete decongestive therapy can help treat include:

- Lymphatic malformations
- Post-cancer treatment edema
- Venous-related edema
- Edema following trauma or injury
- Hereditary conditions
- Congenital lymphatic malformation
- Chronic edema from kidney or heart disease
- Lymphedema-distichiasis syndrome
- Lymphangiodysplasia
While complete decongestive therapy can help a wide range of conditions, it’s often used to manage and prevent the progression of lymphedema. Through a series of treatments, complete decongestive therapy is a non-invasive form of treatment that can help patients regain their quality of life. By working with your lymphedema specialist, they will be able to create a personalized treatment plan that works for you.
How Does Complete Decongestive Therapy Work?
Before you begin complete decongestive therapy, it’s important to have a basic understanding of how it works and what you’re trying to accomplish with CDT. The specifics of your CDT plan may vary depending on your condition and your specialist, but there’s a fairly simple framework that most CDT plans follow. Below is an overview of what you can expect when it comes to complete decongestive therapy.

Phase I: Active CDT
The first phase of complete decongestive therapy is active CDT, which is the stage during which you’ll be working with a lymphedema specialist. Your specialist will create a treatment plan for you that includes regularly scheduled lymphedema treatment ranging from lymphatic drainage to skincare and exercise. The first phase of CDT can be very time-consuming, as your specialist may require you to book sessions anywhere between 1-3 days per week, but could even be up to 7 days during the first week of treatment, depending on the severity of your condition. Phase I can also be expensive, especially if your insurance doesn’t cover all of the costs.
The active stage of complete decongestive therapy can take varying amounts of time depending on how long it takes for the swelling to reduce but can range anywhere between 2-4 weeks. Treatment may also vary based on the severity of your lymphedema. Generally, however, Phase I of complete decongestive therapy includes manual lymph drainage, compression bandaging, exercise, and skincare.
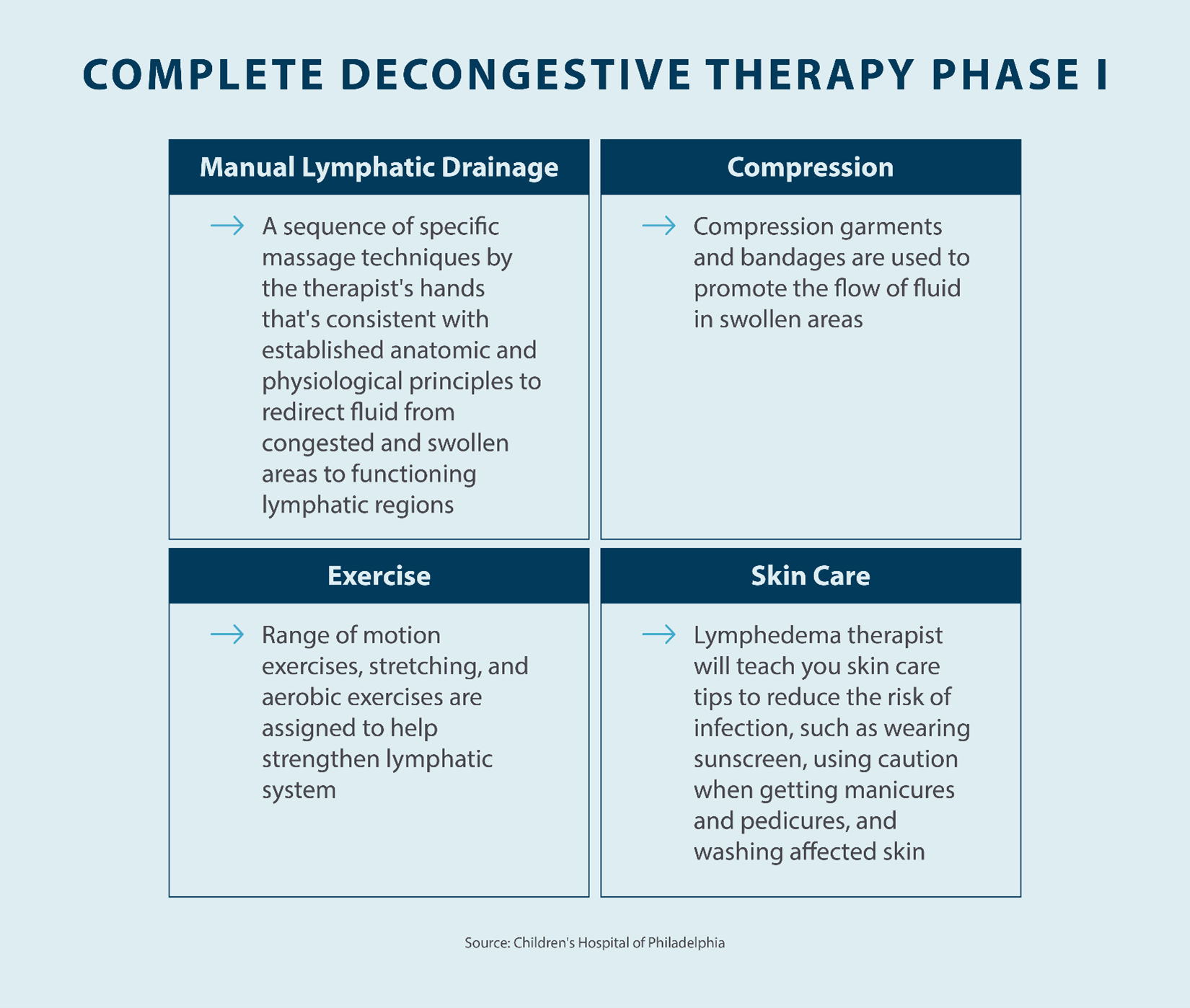
Manual Lymph Drainage
Manual lymph drainage is a technique that’s used to promote drainage in the lymphatic system. With lymphedema, a blockage or malfunction in the lymphatic system can lead to a buildup of fluid in your body’s tissues. In a healthy body, fluid flows smoothly throughout the lymphatic system and back into the circulatory system. However, improper drainage can lead to swelling, pain, skin changes, and other symptoms that come with lymphedema. Manual lymph drainage focuses on encouraging proper drainage through the lymphatic system, and it’s often a major component of lymphedema treatment with CDT. Manual lymph drainage is a simple, non-invasive treatment option that provides benefits for patients living with lymphedema.
One of the primary advantages of manual lymph drainage is that it can be performed at home after direction is given by your lymphedema specialist or doctor. Manual lymph drainage uses a sequence of hand motions, consistent with established anatomic and physiological principles, to redirect fluid from blocked or swollen areas to healthy lymphatic regions. Manual lymph drainage is a key component of complete decongestive therapy and can be a great way to relieve pain and reduce swelling.
During the active phase of CDT, your specialist will perform this massage for you. However, in some cases, patients might not be able to commit to a full in-person treatment plan with their specialist, due to factors like work, finances, transportation, and raising a family. Fortunately, if you don’t have the time to visit a specialist for a lymphatic drainage massage, your specialist can work with you to teach you the proper techniques to use at home.
Compression Bandaging
Compression bandaging is another key component of the first phase of lymphedema treatment. The goal of compression bandaging is to use gentle physical force to help guide lymph fluid out of swollen areas to reduce swelling. Also called multi-layer bandaging, compression bandaging is typically only used in the first phase, as applying bandages yourself can be difficult. If placed incorrectly, symptoms of lymphedema can worsen, which is why your lymphedema specialist or therapist should apply your bandages for you.
With compression bandaging, bandages may be utilized for several weeks, with your specialist removing and reapplying bandages as needed. Multi-layer bandaging often consists of bandages for the toes and fingers, should lymphedema occur on a limb, followed by a tubular bandage, a soft layer of foam, a dense layer of foam, and a top layer of bandages.
Once your bandages are applied by your specialist, you will have to keep them dry, which means covering them when showering or bathing. Additionally, it’s important to clean, dry, and moisturize the skin in between bandage changes to help reduce the risk of infection.
If you’re living with lymphedema, compression bandaging is an important part of relieving symptoms through active complete decongestive therapy. Compression helps relieve swelling, which causes a majority of the symptoms that are present with lymphedema.
Exercise
Exercising is another crucial component of complete decongestive therapy, and making lifestyle changes can help reduce swelling and pain caused by lymphedema. Living a sedentary lifestyle can lead to fluids pooling in certain areas of your body, such as the arms or legs, resulting in lymphedema. However, having a more active lifestyle can help encourage the flow of fluids in your body to reduce swelling, and your specialist will work with you during this phase to teach you exercises and lifestyle changes that you can implement into your daily routine.
When working with your doctor or specialist, they will help create a treatment plan that consists of exercises that can be performed during in-clinic sessions and at home. During clinical sessions, your specialist will typically start off with simple stretches and range of motion exercises to build up your lymphatic system. From there, exercises will progress and include aerobic activities, such as walking, yoga, swimming, or cycling. Your therapist will tailor your physical activity according to your tolerance. Aerobic exercises can help reduce your body weight and improve your general health, which can increase your quality of life.
In most cases, your lymphedema specialist will focus on stretching and aerobic exercises. However, they will typically recommend avoiding weightlifting, as lifting weights can result in swelling. Each exercise plan will be individualized to ensure each patient gets the care they need to manage their symptoms and prevent progression.
Patients who have difficulty walking or a decreased range of motion as a result of lymphedema can still perform basic exercises to help relieve swelling and pain. If your ability to walk is being affected by lymphedema, make sure you talk to your doctor about alternative exercises you can try.
Skincare
While the primary focus of complete decongestive therapy is relieving swelling, pain, and other symptoms, skincare is a crucial component of managing lymphedema symptoms and preventing infection. Swelling that results from built-up fluid can lead to skin problems, including hardening of the skin and ulcers. Patients living with lymphedema often have sensitive, dry, and inflamed skin, which is susceptible to cellulitis and skin injuries. Monitoring the condition of your skin and taking steps to prevent these problems can help you avoid any infections. During this stage, your doctor can advise you about the specific skincare routine you should follow to prevent infections and other lymphedema-related skin problems.
The primary focus of skincare for lymphedema is preventing infection by keeping the skin clean. Best practices to reduce the chance of infection include trimming fingernails and toenails, avoiding needle pricks and small injuries to an edematous area, and keeping the skin clean and moisturized. If you do have a blister, ulcer, or cut on the affected skin, you should thoroughly clean and dry the area before applying a bandage to protect it. If you’re out in the sun, it’s also recommended to protect your skin with sunscreen. Attentive skincare can prevent many of the skin-related issues that may be present with lymphedema.
Ask your specialist about skincare products that may be helpful for people living with edema. Always follow the instructions your specialist provides, especially when it comes to cleaning and moisturizing your skin. Make sure you clean the swollen area on a regular basis and dry the area thoroughly when cleaning is complete. When cleaning, it’s recommended to use a mild, soap-free cleanser with a neutral pH to keep your skin healthy.
Phase II: Maintenance CDT
Once you’ve completed the in-clinic phase of complete decongestive therapy, you’ll move on to Phase II, which is known as the maintenance phase. During this phase, you’ll no longer need to attend in-clinic sessions with your specialist or therapist. Instead, you’ll be responsible for maintaining the results you see from Phase I. Because this phase is focused on maintaining the results you’ve achieved, it’s not uncommon for Phase II of CDT to last for several years or the rest of your life. This includes understanding how to protect your skin from injuries, how to use compression garments to manage swelling and other symptoms over time, and more.
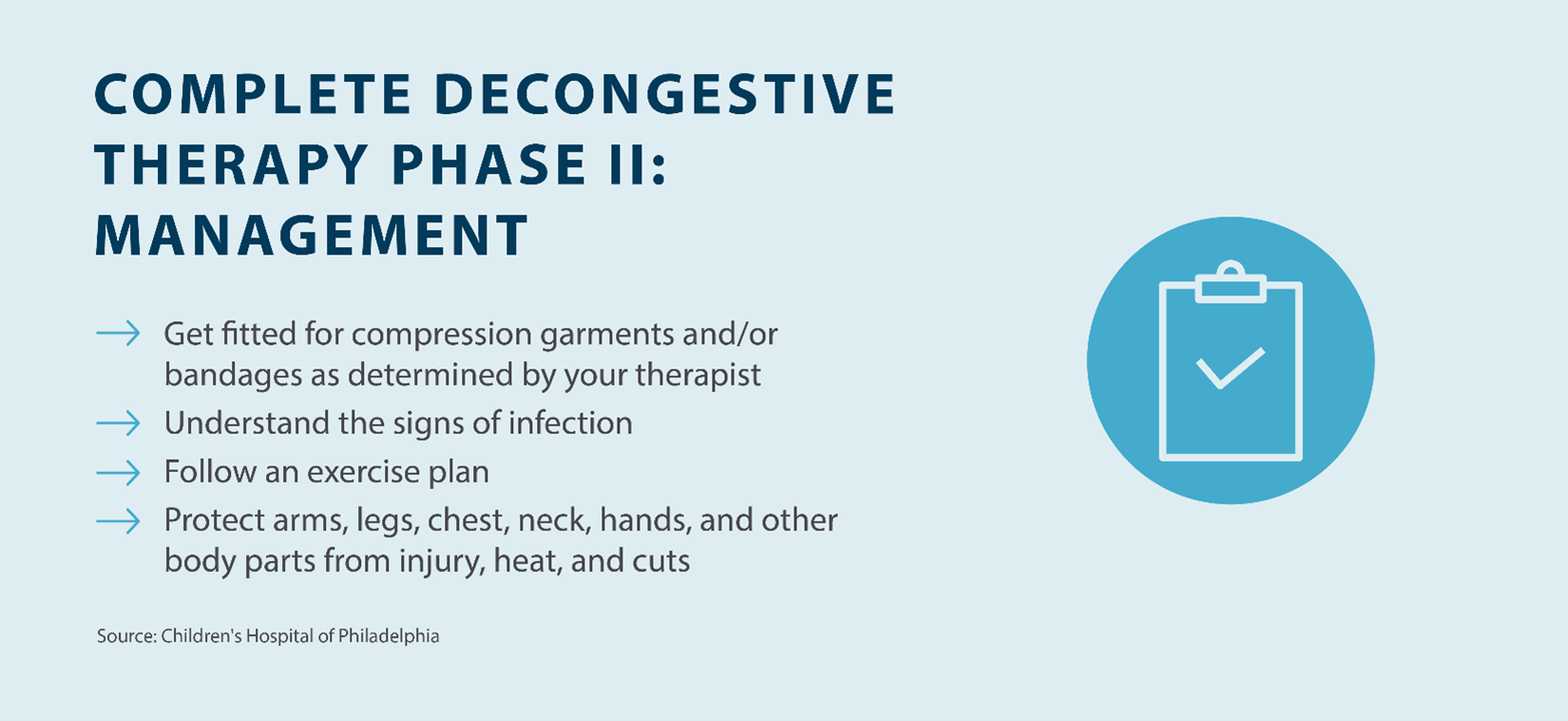
Your specialist may recommend performing regular lymphatic drainage massages at home after you’re done with Phase I of complete decongestive therapy. While there is a technique to perform a lymphatic drainage massage, you don’t need any special tools or devices. Your specialist can teach you how to perform a lymphatic drainage massage and let you know how often you should do them as part of your lymphedema treatment and management plan.
Compression garments are another important part of the maintenance phase of CDT. Once you’ve completed the active phase of CDT, your specialist may recommend compression sleeves, stockings, and other compression garments that encourage the flow of fluid throughout your body. Make sure you talk with your specialist about how to properly wear these garments, as ill-fitting compression garments can lead to further complications.
Exercise is also a crucial component of Phase II of CDT. During this phase, your therapist will provide you with complete decongestive therapy exercises that you can perform at home, such as light stretches and aerobic activities like walking, yoga, or cycling. Maintaining an active lifestyle is essential to managing your lymphedema and preventing its progression.
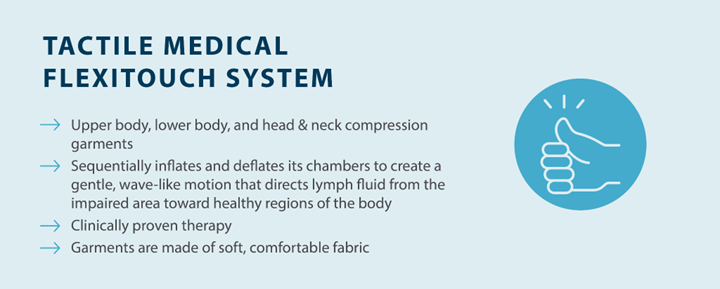
Pneumatic compression devices, such as Tactile Medical’s Flexitouch Plus system, are also a doctor-recommended at-home treatment option that can help maintain your results from Phase I and manage your symptoms. The Flexitouch Plus system is designed for upper body, lower body, and head and neck lymphedema, and works by delivering dynamic pressure in 1-3 second intervals to create a gentle work and release action. These customized treatment options with multiple pressure settings and unique garment designs help direct fluid throughout your body’s watersheds to reduce swelling and pain.
As you spend more time living with lymphedema, you can work with your specialist to make adjustments to your lymphedema management plan based on your triggers and what works for you. If your lymphedema is worse during hot weather, for example, you can incorporate that information into your plan and take extra precautions during the summer. A lymphedema specialist can also help you make adjustments to your lymphedema management plan based on the results you’re seeing and any changes in health.
While the management stage of complete decongestive therapy may seem secondary to the active stage, they’re both crucial parts of the treatment process. Making sure you’re taking care of your skin, using manual lymph drainage, and wearing compression garments to minimize the effects of lymphedema makes it easier to live a healthy and enjoyable lifestyle. As always, consult with your lymphedema specialist before you make any significant changes to your lymphedema management plan.
Key Takeaways on Complete Decongestive Therapy
Complete decongestive therapy (CDT) is a non-invasive treatment option for people who are living with lymphedema, lipedema, and edema. Through a combination of treatment methods, CDT can relieve swelling and offer relief from the symptoms that accompany different forms of edema. Before starting complete decongestive therapy, you should talk to a lymphedema specialist for guidance.
Compression garments are one of several parts of treating lymphedema using CDT. Tactile Medical offers pneumatic compression devices, such as the Flexitouch Plus system, that can help reduce swelling and relieve the pain that comes with lymphedema. To learn more about Flexitouch Plus and how you can incorporate it into your lymphedema treatment plan, talk to your specialist today.