How to Prevent Lymphedema
While there’s currently no way to prevent lymphedema, there are ways to manage the symptoms of this condition. It’s best to talk to your doctor before you make any serious changes. Your doctor can diagnose your lymphedema and help you come up with a treatment plan that works for you and your medical history. Keep reading to learn more about managing lymphedema and lymphedema prevention.
What Is Lymphedema?
What Causes Lymphedema?
Can You Prevent Lymphedema?
How Is Lymphedema Diagnosed?
What Are Lymphedema Treatment Options?
Key Takeaways: Lymphedema Prevention
What Is Lymphedema?
Lymphedema is the accumulation of fluid that results in swelling. Your body’s lymphatic system is responsible for draining the fluid just beneath your skin’s surface to remove toxins and fight infections in your body. However, if there are any disruptions in your lymphatic system, such as a blocked or removed lymph node, that fluid won’t be able to flow, resulting in fluid retention and swelling.
Lymphedema can occur in various parts of the body, though it’s most common for it to affect the legs, arms, hands, and feet. However, it can also affect the head and neck, chest, abdomen, and genitals. Patients with lymphedema may experience chronic swelling, pain, and recurring infections. In some cases, lymphedema may also lead to blisters or ulcers on the skin. Getting diagnosed early and talking to your doctor about lymphedema treatment options can help reduce symptoms, prevent its progression, and improve your quality of life significantly.
What Causes Lymphedema?
There are several causes of lymphedema. While avoiding these causes isn’t always possible, knowing them can help reduce the risk of lymphedema. Here are some of the most common causes of lymphedema:
- Surgery: Lymphedema may be caused by cancer surgery where the lymph nodes are removed to see if they contain cancer. While cancer surgery doesn’t always result in lymphedema, it’s a fairly common side effect.
- Obesity: Adipose tissue, also known as fat, that results from obesity can place pressure on lymph nodes and vessels, which can decrease natural lymphatic drainage resulting in swelling.
- Cancer: Cancer itself can spread to your lymph nodes, at which point it may cause a blockage that results in lymphedema. If this is the case, you should talk to your doctor about your options for relieving lymphedema symptoms and pain.
- Radiation treatment: Radiation can lead to scarring and inflammation in your body, which can also affect the lymph nodes. If your lymph nodes, vessels, or surrounding tissues become scarred or inflamed, they may not be able to carry fluid.
- Trauma: Any trauma to the lymphatic system, such as a crushing injury, burn, car accident, or cut, can damage lymphatic vessels and nodes and cause lymphedema.
- Parasites: In certain tropical countries, lymphedema can be caused by a parasite that can clog your lymph nodes. If you live in a tropical country or have recently visited one, this is something to consider.
If you suspect you may have lymphedema, you should get a diagnosis as soon as possible to find an intervention plan that can help reduce the symptoms.
Can You Prevent Lymphedema?
You may be wondering about lymphedema prevention and whether it’s possible. Unfortunately, there is no way to prevent lymphedema. Because this condition is a result of a lymphatic system damage, there are currently no measures to prevent lymphedema. However, there are several ways you can prevent your symptoms from progressing.
If you’ve had cancer, you can get regular checkups to watch for lymphedema onset, even if you aren’t experiencing the symptoms of lymphedema. This checkup involves taking a measurement of your limbs/body immediately following your cancer treatment, tracking symptoms associated with lymphedema, and following up to make sure that measurement remains consistent.
While it’s normal to experience pain, swelling, and other symptoms following surgery, keeping in touch with your doctor is important. If you experience any sudden changes in your condition or symptoms that appear rapidly, let your doctor know and get a checkup. Changes you may be concerned about include swelling, changes in size, color, skin condition, feel, or temperature.
Maintaining a healthy weight can also help you reduce your risk of lymphedema. Obesity can put you at a higher risk for lymphedema, so maintaining an active and healthy lifestyle is important.
Exercise is one of the most important things you can do when it comes to lymphedema prevention. Exercising regularly helps you regain strength in parts of your body that have been affected by cancer, plus it helps you maintain a healthy weight. Exercise can also promote the drainage of lymphatic fluid, which is an excellent way to relieve swelling associated with lymphedema. If you have lymphedema, it’s important to talk to your specialist or a trained fitness expert to determine an appropriate exercise plan that works for you. It’s recommended to start slow and work your way up to more intensive exercises to avoid further complications with your lymphedema.
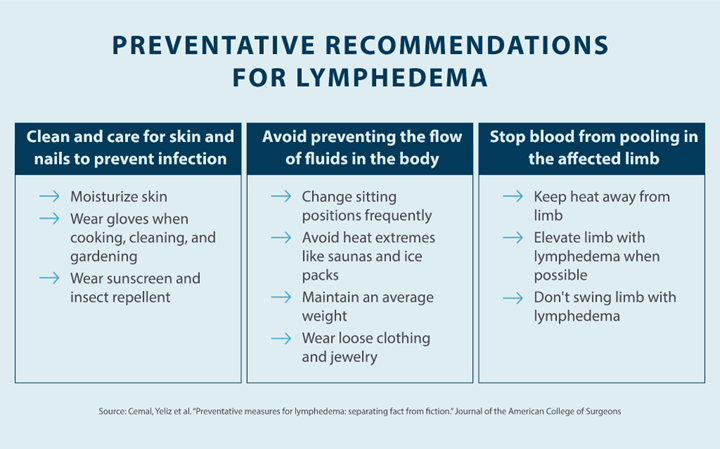
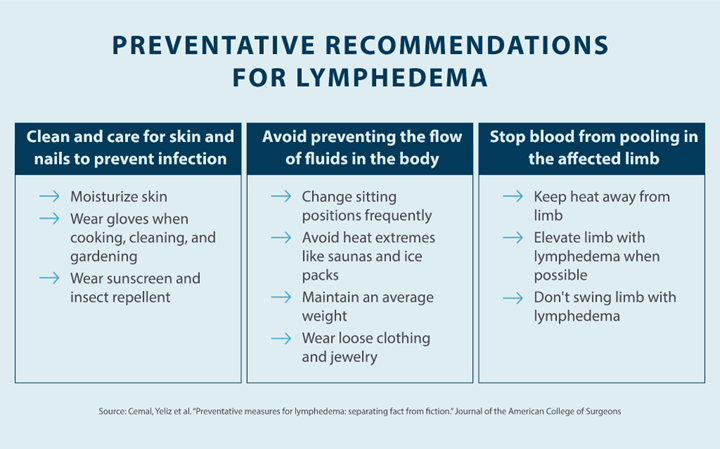
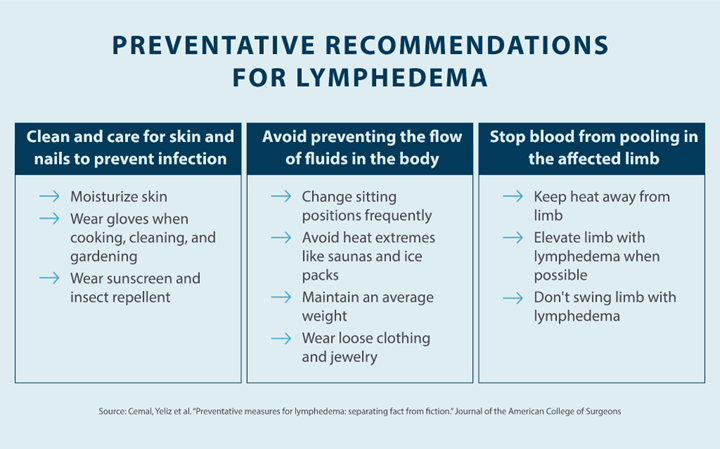
When your skin is injured, whether from a burn, cut, or infection, your body sends white blood cells and fluid to the injured area. For people living with lymphedema, any skin injuries can lead to infection, so it’s important to practice safe hygiene. This means trimming your fingernails safely, using sunscreen, wearing gloves when gardening or cooking, and using an antibiotic ointment on any cuts you may have.
It’s also recommended to avoid needle pricks. If you want to sew, make sure you’re using a thimble. As far as vaccinations, blood pressure gauges, and blood draws go, it’s often advised to avoid the affected limb and to use a body part that isn’t affected by lymphedema.
Avoiding tight clothing, jewelry, and shoes can also help you reduce your risk of lymphedema. Anything tight on your body can decrease lymphatic drainage, so wear looser, more comfortable clothes and shoes. It’s also recommended to elevate any body parts affected by lymphedema to encourage the flow of fluid and reduce swelling.
How Is Lymphedema Diagnosed?
In order to diagnose lymphedema, a specialist will look at your medical history, perform a physical examination, and use imaging tools. Below is a breakdown of what a specialist will typically do to diagnose lymphedema.
When reviewing your medical history, your doctor or specialist will typically consider the onset of symptoms first. Depending on when the swelling began, a specialist may be able to determine the likely cause of your lymphedema. They’ll also look at any injuries you may have had that could have caused lymphedema. Your specialist may also ask if your parents have swelling in their extremities, as genetics can play a role. Doctors will also look at your symptoms to make sure it’s lymphedema and not another medical condition.
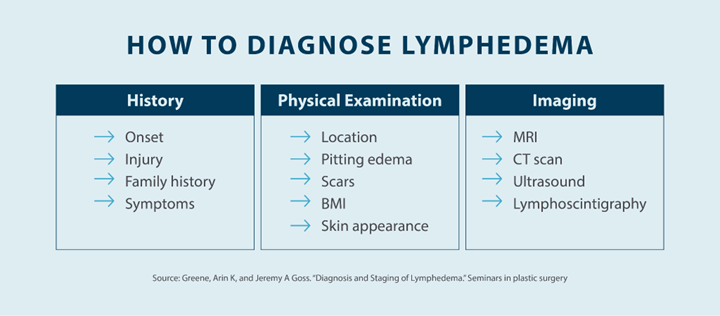
During the physical examination, your specialist will consider the location of your lymphedema and look for pitting edema, which is characterized by an indent left on the affected area after pressure is applied. Your Stemmer sign, or whether or not the area can be pinched, will also be factored in, as will your BMI. Your doctor will also use your skin condition to help diagnose lymphedema.
A specialist may also use several imaging tools to help diagnose lymphedema, including MRI, CT scan, ultrasound, and lymphoscintigraphy. Ask your specialist to learn more about these tests, what they show, and how they work.
What Are Lymphedema Treatment Options?
As far as lymphedema treatment and management go, there are several options at your disposal. Managing your weight, performing lymphatic drainage massages, and wearing compression garments are all recommended actions you can take to manage your lymphedema symptoms.
Your doctor can also prescribe pneumatic compression devices, such as those offered by Tactile Medical. Our Flexitouch Plus system is specifically designed to provide compression to relieve lymphedema symptoms. If you’re experiencing pain and swelling as a result of lymphedema, these devices can help stimulate your lymphatic system to encourage drainage. Flexitouch Plus is available for your lower body, upper body, and head and neck. Our at-home lymphedema treatment systems allow you to find relief in the comfort of your home to enjoy a better quality of life.
Key Takeaways: Lymphedema Prevention
While there are no proven lymphedema prevention plans, regular checkups, maintaining a healthy weight, and regular exercise can help reduce your risk of lymphedema. If you’re living with lymphedema, you can talk to your doctor about potential treatment options, including massages and garments.
If you’re looking for relief from lymphedema, Tactile Medical can help. Our Flexitouch Plus system can help stimulate your lymphatic system, and it works for every part of your body. Review our Flexitouch Plus system to learn more about our doctor-recommended treatment options and how they can help with the self-management of lymphedema.