Measuring Edema
How to Measure Edema
Measuring edema is a crucial step in keeping an eye on your symptoms and managing your edema. Edema assessments should be a routine part of your edema management plan, as it allows you to monitor your edema to better understand its severity and what your best treatment options are. Routine edema measurements can also help you prevent your edema from worsening over time. If you want to know more about how to measure edema and what you can do to manage your symptoms, review our guide below.
What Is Edema?
What Causes Edema?
How Is Edema Assessed?
History Assessment
Physical Assessment
How Do You Measure Edema?
Edema Measurement Chart
Can You Treat Edema?
Manage Edema Symptoms at Home With Tactile Medical
What Is Edema?
Edema is a medical condition that’s caused by a buildup of excess fluid in the body tissue. Edema can occur in any part of the body but is most common in the hands, arms, feet, ankles, and legs. This swelling can lead to various symptoms, including pain, skin that feels stretched or appears shiny, and swelling in the affected area. In some cases, you may have pitting edema, which is a type of edema characterized by dents or pits left in the skin after pressure is applied.
While edema may not present a serious risk at first, it can eventually progress to the point that it causes serious complications. For example, if acute edema is left untreated, over time, it can lead to lymphedema. If you’re diagnosed with edema, you should talk to a doctor about reducing swelling and preventing edema complications. Lifestyle changes and at-home treatment can help prevent complications and allow you to maintain your quality of life.
What Causes Edema?
Understanding the causes of edema and how to perform an edema assessment are important parts of preventing its progression and managing symptoms. Edema is caused when blood vessels in your body leak fluid into the surrounding tissue, and the lymphatic system is unable to absorb this fluid effectively. Here are some of the potential causes of edema that you should keep in mind:1

- Hot weather: Edema that’s caused by hot weather is known as heat edema, which is a result of the way heat affects your blood vessels. Hot weather can lead to the expansion of blood vessels, which can cause blood to accumulate in the legs or arms.
- Blood clots: Blood clots interrupt the flow of blood in your circulatory system, which can lead to edema in the area of the body near the clot. Superficial blood clots that are caused by a recent injection or IV line aren’t typically a cause for concern, but deep vein thrombosis can be a life-threatening condition. If you notice swelling that you think may be the result of DVT, you should go to the hospital immediately.
- Venous insufficiency: Chronic venous insufficiency is a medical condition characterized by damaged valves inside the veins. When these valves are damaged, they’re unable to push blood against the force of gravity and back up toward the heart. The result is blood pooling in the lower extremities, which can lead to edema.
- Congestive heart failure: Heart failure can lead to cardiovascular damage that causes edema. Damage to the cardiovascular system can make it more challenging for fluids to flow throughout the body, and these disruptions to the flow of fluid can lead to edema.
- Obesity: Obesity can put stress on your body, and that includes your cardiovascular system. The additional stress on your cardiovascular system caused by obesity can eventually lead to edema, especially if you live a sedentary lifestyle.
- Medications: Certain medications can cause complications with your cardiovascular system that may lead to edema, such as NSAIDs like ibuprofen, birth control pills, and corticosteroids. Make sure you talk to your doctor about the potential side effects and complications of any medications you’re taking.
- Liver or kidney disease: As liver and kidney disease progress, they can cause damage to your cardiovascular system, which can lead to edema. Like congestive heart failure, it’s important to work with a doctor or specialist to manage symptoms and prevent complications if you have liver or kidney disease.
How Is Edema Assessed?
A routine edema assessment can help you avoid treating edema blisters and other potential symptoms of edema. When diagnosed with edema, your doctor will perform an assessment to determine the severity of your edema. Physicians use a history assessment as well as a physical assessment to measure edema. We’ll take a closer look at how those assessments work below.
History Assessment
History assessments can help your physician understand when you first noticed edema symptoms and what may have caused your edema. By understanding your medical history and the onset of your edema, physicians can get a better understanding of how to treat and manage your condition. Here’s how history assessments work:1
- Onset of edema: Your physician will start by asking about when you first noticed edema symptoms to get a better understanding of the progression of your edema and how severe it may be.
- Medication history: Certain medications can lead to edema or increase your risk of developing edema, so your physician will want to know about any medications you take.
- Medical history: By looking for potential causes of edema, such as chronic venous insufficiency, blood clots, and liver or kidney disease, your physician can better determine what might have caused your edema.
- Family history: Your genetics may play a role in your risk for edema, so make sure you mention your family history and whether your parents or grandparents had similar medical issues.
- Diet: You’ll also talk about your diet to rule out any potential dietary choices that may be worsening your edema. Your doctor may also recommend dietary changes based on your current diet.
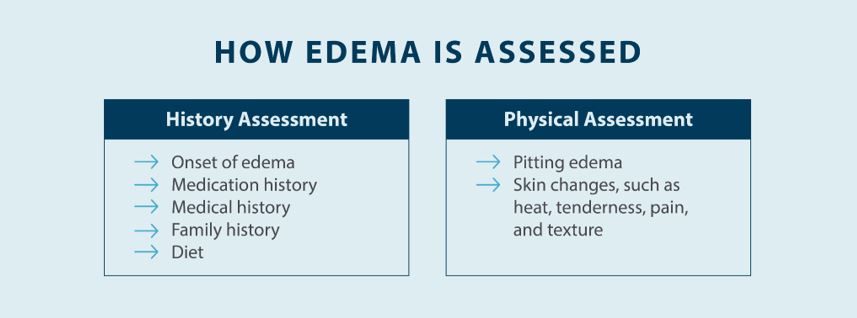
Physical Assessment
The next step is performing a physical assessment to determine the severity of the swelling. Understanding your medical history helps your physician understand how long you’ve had edema and what your best treatment options may be, but performing a physical assessment to get an edema measurement is essential. Here’s what your physician will do to physically assess your edema:1
- Pitting edema: Pitting edema is when you can apply pressure to the swollen area to create a pit, and that pit remains for more than a brief moment. Your physician can test for pitting edema by simply pressing a finger into your skin and looking at the depth of the indentation as well as how long the indentation remains. Pitting edema is graded on a scale from 1-4.
- Skin changes: Because edema causes swelling, it can also affect your skin in the swollen areas. You may notice pain or a warm feeling where edema occurs, and there may also be changes in the texture and appearance of your skin. Your physician will look at your skin to help determine how severe your edema is.
How Do You Measure Edema?
Measuring edema is a vital part of determining the best treatment plan and taking steps to manage symptoms, such as implementing complete decongestive therapy. Your edema measurement will help determine what kind of treatment plan is right for you, and it will also help you figure out whether your edema is progressing or not. If you want to know more about how to measure edema and what the different edema measurements mean, here’s how each measurement is taken:
- Measuring volume: Volume is an important edema measurement, and one easy method for measuring volume is through a water displacement test. With a water displacement test, you place your foot into a container of water that has a spout right near the water line. When you place your foot in this box, the water your foot displaces goes through the spout and is collected in a graduated cylinder. This test can also be used to measure the volume of the hands and ankles. This test is one of the most effective ways to assess edema, but it’s also one of the more time-consuming tests because you have to wait for the water to stabilize in the container.2
- Measuring girth: Girth is the measurement around area of your body, such as your foot, ankle, thigh, upper arm, chest area, or hand, and it can be determined in two ways. The circumferential method involves wrapping a soft tape measure around the swollen extremity to measure the circumference. The figure-of-eight method is another method of measuring the circumference, which is more effective for larger areas. This girth measurement technique is often used for ankle and hand swelling. Your physician may use one or both of these girth-measuring techniques depending on the location and severity of your edema.2
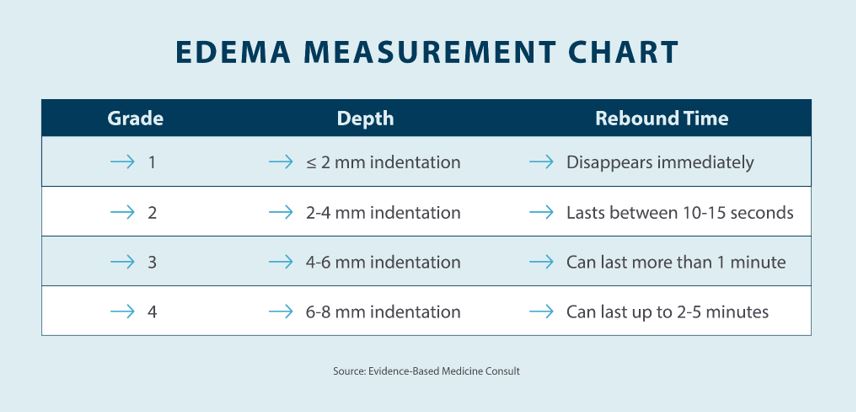
- Assessing pitting edema: Assessing pitting edema is as simple as using a finger to press down on the swollen area and examining the depth of the indentation. You can press your hand over the dorsum of the foot, behind the medial malleolus, or on the lower calf above the medial malleolus, according to edema assessment guidelines. After you remove your finger from the indented area, you can look at the depth of the indentation, as well as the time of how long the indentation remains. Pitting edema is graded on a scale of 1-4 depending on the time the pitting lasts, as well as the depth of the indentation.2
Edema Measurement Chart
Now that you understand the basics when it comes to assessing and measuring edema, you might be wondering what those edema measurements actually mean. When you visit a doctor or specialist, you should figure out the volume and girth of your edema as well as the grade of your pitting. You can find out more about what each of these numbers means in the edema measurement chart below.3
Can You Treat Edema?
One of the challenges of living with edema is that it’s not always easy to treat. Treatment for edema depends on the cause of your edema, which is why it’s so important to visit a professional for an edema assessment. Your physician can help you determine the cause and severity of your edema and help you create a treatment plan that works for you. Here are some of the edema treatment options your physician may recommend:
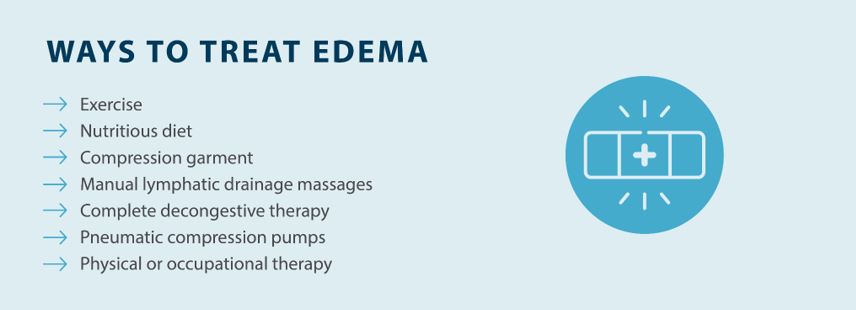
- Exercise: Losing weight can reduce the stress on your cardiovascular system and relieve edema symptoms. Additionally, exercising is also important if you’re at a healthy weight, as exercise is still very beneficial for managing edema and reducing swelling. If you have severe edema, talk to your doctor about exercising safely before you get started.
- Nutritious diet: A healthy diet can help you improve your heart health and lose weight, which are both essential when it comes to treating edema. Foods high in salt can result in higher water retention in the body, which can lead to swelling.
- Compression garments: Compression garments for lymphedema and edema can reduce swelling in the affected extremities to help prevent edema from progression. Compression can help improve circulation, allowing fluids to move easier throughout your body.
- Manual lymphatic drainage massages: Manual lymphatic drainage massages can reduce edema and lymphedema swelling by encouraging the flow of lymph, especially in damaged areas of the lymphatic system.
- Complete decongestive therapy: Complete decongestive therapy is a combination of treatments used to treat edema, including compression garments, manual lymphatic drainage, skin and nail care, and exercise.
- Pneumatic compression pumps: Pneumatic compression devices gently compress the swollen areas to relieve swelling and encourage the flow of lymph, which helps you get relief from symptoms and prevent edema complications.
- Physical or occupational therapy: You can also work with a physical therapist to relieve edema through exercising, stretching, and other activities. This can be a great choice if you’re having trouble exercising with edema symptoms.
Manage Edema Symptoms at Home With Tactile Medical
Measuring edema is a crucial part of figuring out how severe your edema is and how you should treat it. Your physician can also help you determine the potential cause of your edema with a history assessment. When it comes to getting relief from edema, Tactile Medical can help with our Flexitouch Plus System. With the Flexitouch Plus System, you get targeted relief from edema thanks to pneumatic compression, and there are devices available for your lower body, upper body, and even your head and neck. Try the Flexitouch Plus System from Tactile Medical and get the edema relief you deserve at home.
Sources:
1. Trayes KP, Studdiford JS, Pickle S, Tully AS. Edema: diagnosis and management. American Family Physician. 2013;88(2):102-10. https://www.aafp.org/pubs/afp/issues/2013/0715/p102.html
2. O’Sullivan, S.B. and Schmitz T.J. (Eds.). (2007). Physical rehabilitation: assessment and treatment (5th ed.). Philadelphia: F. A. Davis Company. p.659 https://geriatrictoolkit.missouri.edu/cv/pitting_edema.html
3. Busti, Anthony J. Pitting Edema Assessment. Evidence-Based Medicine Consult. 2016. https://www.ebmconsult.com/articles/pitting-edema-assessment