Should I Use Compression Garments for Lymphedema?
When it comes to treating lymphedema, getting relief from your symptoms and preventing progression or worsening of this condition is the best thing you can do. Compression garments are a standard treatment option if you’re looking for a simple way to reduce swelling and some of the symptoms that come with it. While this can be an effective treatment method, it’s best to talk to your doctor before trying compression garments for lymphedema. There’s not one-size-fits-all solution.
This article will describe what lymphedema is and the symptoms. We’ll also discuss compression garments as a lymphedema treatment option, including the pros and cons and how you can decide if compression garments are right for you.
What Is Lymphedema?
What Are Signs of Lymphedema?
What Are Compression Garments for Lymphedema?
How Do Compression Garments for Lymphedema Work?
What Is Compression Bandaging?
Does Insurance Cover Compression Garments for Lymphedema?
Wrapping Up: Compression Garments for Lymphedema
What Is Lymphedema?
Lymphedema is a condition characterized by swelling that occurs as a result of a buildup of fluid. This buildup occurs when there is a disruption in the body’s lymphatic system, which is responsible for transporting toxins and fighting infections. The fluid that flows through the lymphatic system consists of fat, water, protein, cellular debris, and white blood cells. However, a disruption in the lymphatic system, such as a clogged or damaged lymph node, can cause lymphatic fluid to build up in the body’s tissues.
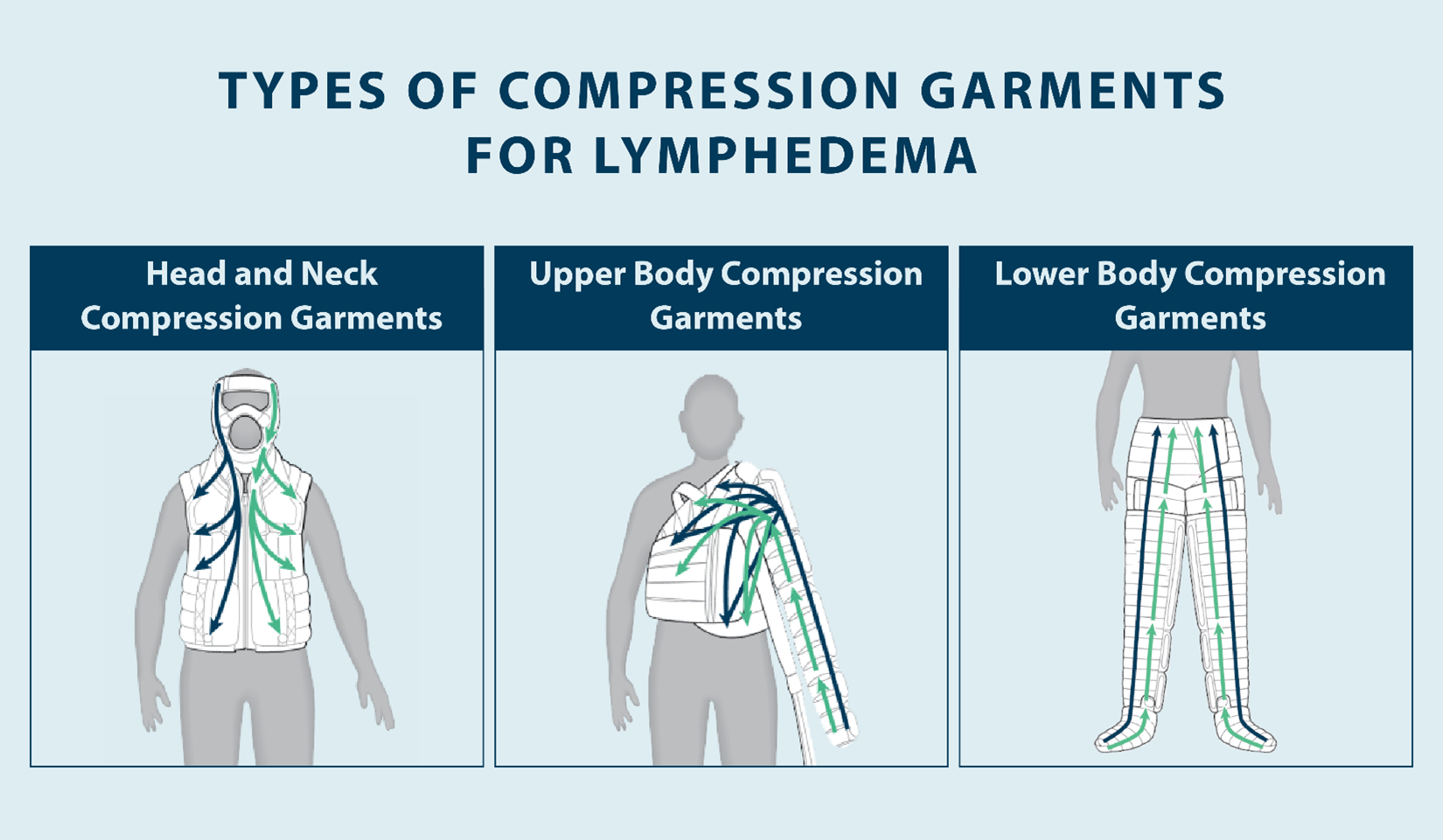
Lymphedema can be classified as primary or secondary. Primary lymphedema is lymphedema that’s caused by a lymphatic system issue that’s present at birth or inherited, while secondary lymphedema is the more common form. Secondary lymphedema can occur as a result of cancer, cancer treatment, chronic venous insufficiency, physical trauma, obesity, and more.
There are a handful of risk factors for lymphedema, so getting a professional diagnosis is important. Your doctor can help you determine the best treatment plan for your lymphedema, including whether compression garments are a safe treatment option for you. In many cases, lymphedema treatment is focused on stimulating the lymphatic system to drain excess fluid and finding relief from your symptoms.
What Are Signs of Lymphedema?
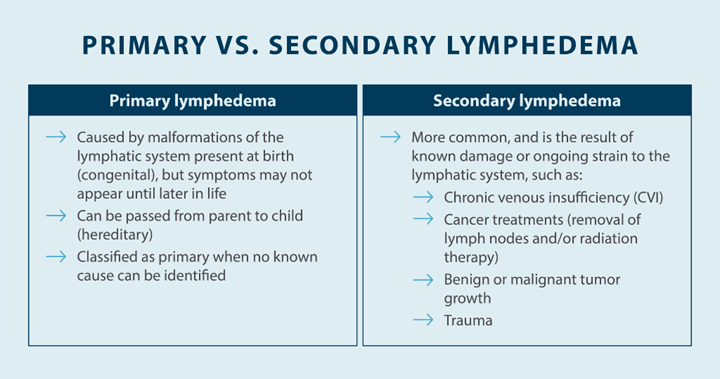
The earlier you’re diagnosed with lymphedema, the easier it can be to treat. Symptoms of lymphedema can progress over time if you neglect treatment, so it’s important to talk to your doctor as soon as possible to get a diagnosis and start a treatment plan. Here are some of the signs and symptoms of lymphedema:
- Heavy limbs: As lymphatic fluid begins to pool up in your arms and legs, it can lead to swelling and cause your limbs to feel heavier. Reducing swelling can help reduce the sensation of heaviness in your limbs, whether you elevate the affected limb or use compression garments to help stimulate your lymphatic system.
- Aching, fatigued limbs: Swelling in your limbs due to lymphedema can also cause aching, fatigued limbs. Without proper treatment, this symptom can worsen and affect your quality of life.
- Pitting: Pitting is when you can press down on skin affected by lymphedema and your finger leaves an indent. Pitting is graded based on how deep of an indent your finger leaves in your skin and how long it takes for that skin to bounce back to its original shape.
- Swelling: Swelling is the most common sign of lymphedema, and it causes or exacerbates many of the other symptoms. Reducing swelling is a primary focus when it comes to treating edema, which is why getting a diagnosis and treatment plan is important.
- Loss of range of motion: When your limbs are swollen, it can affect your ability to move your joints freely. You might experience a loss of range of motion in some of your limbs as a result of lymphedema. This symptom can usually resolve itself when you find a way to reduce swelling.
- Loss of mobility: While the pain, stiffness, and loss of range of motion that comes with lymphedema are minor for some patients, they can cause a loss of mobility for others. A loss of mobility can make It difficult to walk due to painful swelling.
- Skin changes: Lymphedema can lead to a handful of skin problems, including skin infections, fibrosis, hardening of the skin, and more. To prevent the risk of infection, take proper care of your skin by avoiding cuts, scrapes, and needle pricks, wearing sunscreen, and washing your skin.
- Loss of muscle strength: Because lymphedema can make it difficult to use your joints and muscles regularly, you can also suffer a loss of muscle strength over time as a result. If you’re not walking around often or moving your arms and legs like you normally would, they can get weaker.
- Ulcers: Ulcers can occur on the skin as a result of lymphedema, so it’s important to take good care of your skin to prevent infection.
- Stemmer sign: If the skin in an edematous area such as the hand or foot can’t be pinched, that’s a sign that you may have lymphedema. Your doctor will perform other tests to rule out any other possible medical conditions.
- Pain: Swollen legs, arms, hands, and feet can eventually become painful. Pain that results from lymphedema is different for everybody, and some people don’t feel pain from this condition. If you’re experiencing pain, it’s likely a direct result of the swelling.
- Dysphagia: Certain forms of lymphedema may cause dysphagia, or difficulty swallowing. If you’ve noticed it’s been hard for you to swallow even when eating and drinking, that could be a sign of lymphedema in the head or neck.
Some of the symptoms of lymphedema may also be present with edema that’s not related to your lymphatic system. Monitoring your symptoms is an important part of diagnosing lymphedema and deciding on the best treatment for you.
What Are Compression Garments for Lymphedema?
Compression garments for lymphedema are a treatment option that involves wearing specialized clothing that compresses your skin to promote the flow of fluids and increase circulation. A doctor or lymphedema specialist can prescribe these garments to help you manage and live with lymphedema. Compression stockings are one of the most common types of compression garments, and you can find compression arm sleeves, socks, bodysuits, and more.
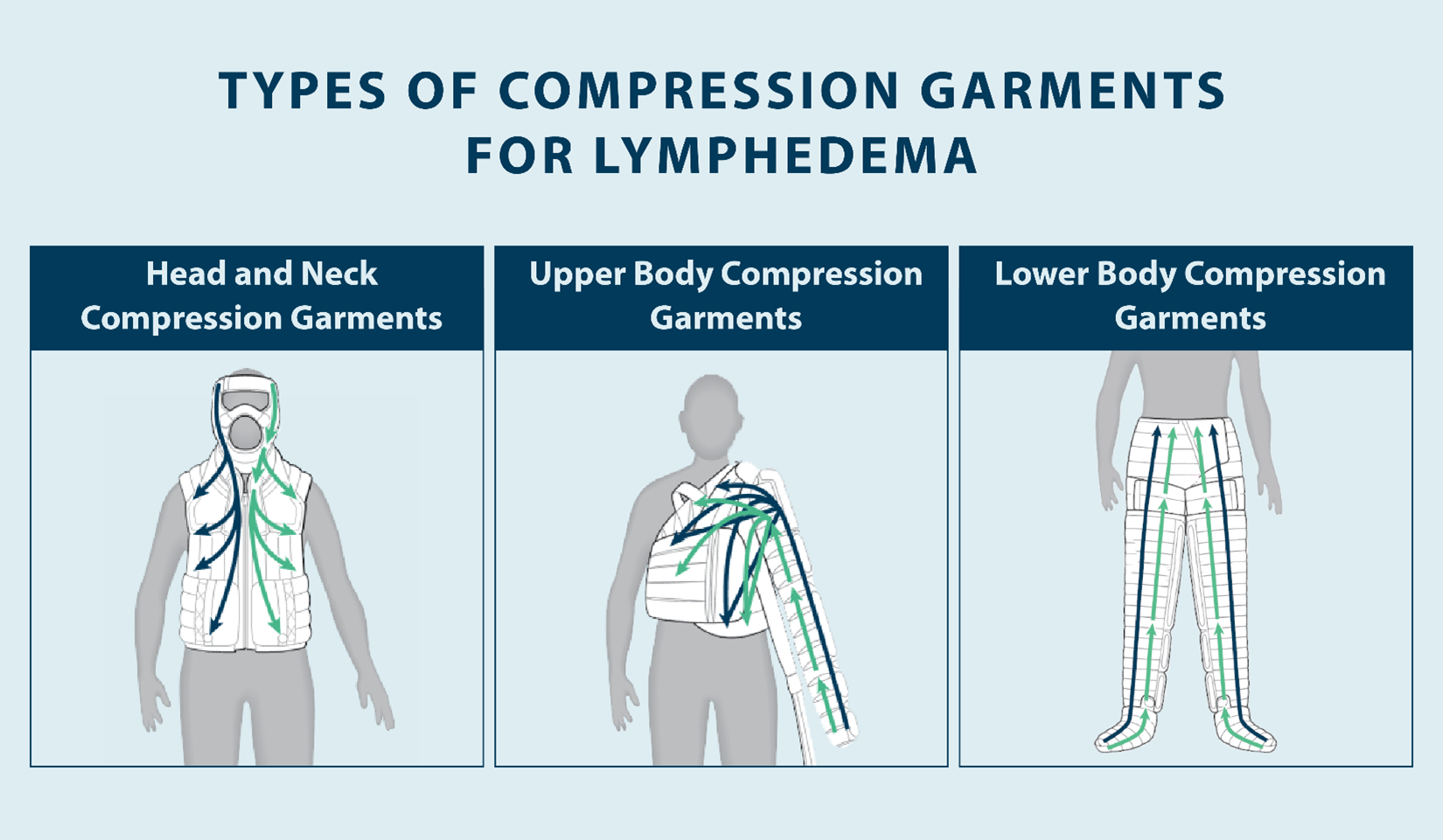
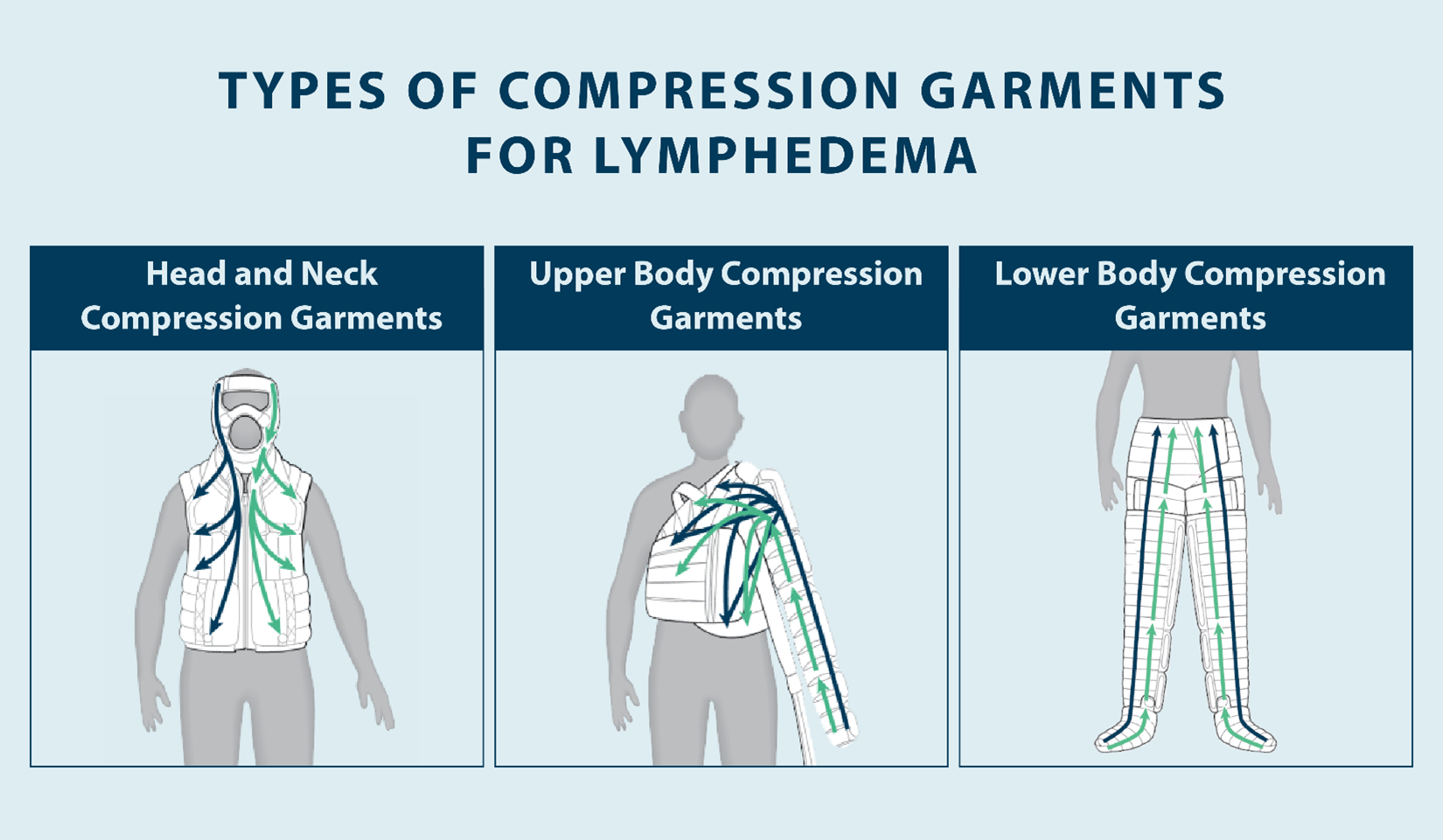
It’s important to keep in mind that standard compression garments aren’t the only forms of compression therapy. Compression therapy can also be administered with multi-layer bandaging systems and pneumatic compression devices. The Flexitouch Plus system from Tactile Medical is an example of a pneumatic compression device that can help stimulate your lymphatic system. If you do not see results with compression garments alone, Flexitouch Plus may be the right lymphedema treatment option for you. At Tactile Medical, we offer lower body, upper body, and head and neck lymphedema garments that can be worn in the comfort of your home to help manage symptoms and help improve your quality of life.
There are a few guidelines to follow when wearing compression garments, so make sure you talk to your specialist. Keeping your compression garments clean is important for skin health, and you shouldn’t wear compression garments that are designed for daytime use while you sleep.
Your doctor may recommend compression garments for lymphedema in addition to basic lifestyle changes and exercises. While compression garments can help reduce swelling, you can implement other treatment options into your routine to manage your symptoms. Your specialist may recommend regular exercise, manual lymph drainage massage, and other techniques designed to reduce swelling, in addition to wearing compression garments.
How Do Compression Garments for Lymphedema Work?
The purpose of compression garments for lymphedema is to stimulate the lymphatic system to encourage the movement and drainage of lymphatic fluid. These devices work using gradual sequential compression, which helps push fluid in a certain direction by gently applying gentle pressure to your skin in various parts of your body. For example, lymphedema compression sleeves for legs can help you get relief from some of the pain and swelling in your lower body.
Some compression garments are pneumatic instead of using graded compression, such as the Flexitouch Plus system from Tactile Medical. Instead of using graded compression created by tight garments, these devices use air to create pressure that squeezes your body gently, which can help reduce swelling and encourage the flow of lymph fluid throughout your lymphatic system. Clinical studies have shown the Flexitouch Plus system to be the most effective form of relief compared to conservative therapy or other compression pumps.
One of the main benefits of compression garments for lymphedema is to prevent swelling after you go through bandaging. When using compression garments to prevent swelling, it can help improve your range of motion and help you improve your quality of life.
When choosing compression garments for lymphedema, there are a few factors to consider when. First, compression garments fit very tightly, which means if you’re sensitive to tight clothing or have blisters or ulcers, you may need an elastic Velcro strap bandaging system.
Additionally, compression garments can be susceptible to bacterial growth if not taken care of properly. If you’re wearing compression garments, wash them regularly to prevent the occurrence of skin infections.
What Is Compression Bandaging?
Compression bandaging is an effective therapeutic technique that uses multiple layers of short stretch bandages to stimulate your lymphatic system to reduce excess fluid and facilitate increased flow and drainage of lymph fluid.

With compression bandaging, you need to have your bandaging applied by a lymphedema specialist at first. However, most therapists will instruct the patient in self gradient compression bandaging so they can apply bandages themselves at home, and many do this every night on their own. Daily bandaging may be part of intensive treatment for lymphedema, and that bandaging may be accompanied by lymphatic drainage massages.
When applying compression bandaging, a specialist will use different types of bandages in multiple layers to create compression on the affected limb. This bandaging may include a soft foam layer, a dense foam layer, and multiple layers of bandaging. Some newer products include both the foam and compression bandaging in one layer, which can reduce the amount of time compression bandaging takes to apply.
Once you’ve had compression bandaging applied, you need to follow therapy instructions when it comes to bathing and showering. If you’re going to take a bath or shower at home, you need to make sure you’re covering up your bandaging. Water can affect the compression these bandages provide and can encourage bacterial growth underneath the bandaging. In some cases, you may be able to take a shower in between compression bandaging applications. If that’s the case, make sure you thoroughly dry and moisturize your skin after you’ve showered but before you have new compression bandaging applied.
Because compression bandaging can be cumbersome, it’s recommended to wear loose fit clothing when bandaged. Your doctor or specialist may provide instructions for exercises you can do to help reduce swelling and stimulate your lymphatic system; make sure you’re doing these exercises on a regular schedule.
You should only apply compression bandaging under the supervision of a lymphedema specialist because without proper training it can be dangerous. There are certain types of bandages that are used for gradient compression. When applied by a specialist, compression bandaging can be an effective form of lymphedema treatment.
Does Insurance Cover Compression Garments for Lymphedema?
One factor to consider is whether or not your insurance will cover your treatment. Medical-grade compression garments for lymphedema can be an investment. Fortunately, most insurance companies can help cover the costs of compression garments for lymphedema.
Tactile Medical works with health insurance plans to get coverage for effective lymphedema treatment option that offers an alternative to standard compression garments. The Flexitouch Plus system is covered by Medicare, Veterans Affairs, and many private health care plans.
Our reimbursement specialists have an efficient process to work with patients, their doctors, and their health care providers to ensure they get insurance coverage for at-home treatment to manage lymphedema symptoms.
In most cases, your insurance company will provide coverage for compression garments as long as they’re used to treat a qualifying medical condition, such as lymphedema. However, some patients may have a hard time getting reimbursed for compression garments. Our team at Tactile Medical focuses on customer service and patient advocacy to ensure you can get your quality of life back.
Before you decide on a treatment option for your lymphedema, you should talk to your specialist and your insurance company to determine the cost and what insurance will cover. Consistency is important with lymphedema treatment and management, so it’s best to find a treatment option that you can afford to stick with.
Wrapping Up: Compression Garments for Lymphedema
Lymphedema is a chronic condition that is characterized by the disruption in the lymphatic system that results in fluid retention and swelling. In some cases, primary lymphedema can be inherited or present at birth, while secondary lymphedema is more common and can be the result of factors like cancer or cancer treatment. Compression garments are one of many treatment options your doctor may recommend to reduce swelling and relieve lymphedema symptoms. Compression garments place static pressure on the area affected by lymphedema to reduce fluid accumulation, increase circulation and promote the flow of fluid.
Pneumatic compression devices, such as Flexitouch Plus from Tactile Medical, can provide an alternative to traditional compression garments for people living with lymphedema. These devices are available for the lower body, upper body, and head and neck, and provide a gentle stretch and release technique to reduce swelling and pain. If you’re ready to regain control of your life and manage your symptoms at home, talk to your lymphedema specialist to learn more about Flexitouch Plus and whether it’s right for you.