Lymphedema and Weight Loss
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More

Lymphedema is most common in your arms and legs, but that doesn’t mean it can’t affect other parts of your body. Lymphedema in feet can have significant impacts on your daily life, making it difficult to walk and perform other simple tasks. Learning about the symptoms and causes of lymphedema in feet can make it easier to manage your symptoms and maintain your quality of life. You can learn more about lymphedema in feet, what causes it, and how to treat it below.
What Is Lymphedema?
Can You Get Lymphedema in Your Feet?
What Are Symptoms of Lymphedema in Feet?
How Is Lymphedema in Feet Diagnosed?
What Is the Treatment for Lymphedema in Feet?
Wrapping Up: Lymphedema in Feet
Lymphedema is a medical condition that causes swelling as a result of built-up fluid in your tissues. In a healthy body, fluid flows through your lymph vessels and nodes before returning to your bloodstream, but a blockage or damage can cause fluid to build up in the area. This buildup of fluid can accumulate in the surrounding tissue and cause swelling, which is the primary symptom of lymphedema. While lymphedema mostly affects the arms and legs, lymphedema in feet and other areas is also a possibility.
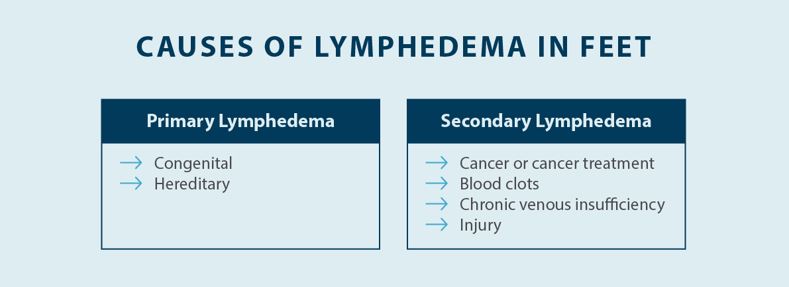
There are two distinct types of lymphedema — primary lymphedema and secondary lymphedema. Lymphedema that occurs as a result of genetics, known as hereditary lymphedema, or lymphedema that is congenital and present at birth, is considered primary lymphedema. However, primary lymphedema symptoms can take several years or even decades to present, and there are different names for it depending on the onset of symptoms. The more common type of lymphedema is secondary lymphedema, which can be caused by cancer and cancer treatment, an acute injury, disease, or another factor that’s unrelated to genetics.
The causes of primary lymphedema can be challenging to identify. Primary lymphedema is thought to be linked to a several gene mutations, such as a genetic mutation involving the FOXC2 gene, leading to lymphedema that typically develops during or after puberty, which is also known as lymphedema praecox.1 In some cases, people with primary lymphedema don’t experience swelling and other symptoms until they’re over the age of 35, which is known as lymphedema tarda.2 While there’s no exact known cause of primary lymphedema, research suggests that genetics may play a role. However, classification of primary lymphedema moving away from solely classifying primary lymphedema based on the age of onset to a classification system that involves phenotyping, called St. George’s Classification Algorithm of Primary Lymphatic Anomalies.3
Secondary lymphedema has many potential causes. Secondary lymphedema can be caused by cancer, cancer surgery, or radiation therapy. Cancer that affects your lymphatic system or leads to lymph node removal can cause a disruption in your lymphatic system, leading to swelling in the affected area. In patients who haven’t had cancer, lymphedema can be caused by chronic venous disease, acute injuries to the lymphatic system, infections, and certain disease or medications. There are also several risk factors for lymphedema, including obesity and prolonged sitting or standing.
Getting a diagnosis is an essential part of treating lymphedema because there are so many different types and potential causes. Reducing swelling and reducing the progression of symptoms is a primary focus in managing lymphedema. If you have symptoms of lymphedema in your feet or any other area of your body, it’s recommended to schedule an appointment with your doctor.
Lymphedema most commonly affects the arms and legs, but it can also affect the feet and other areas like the groin, abdomen, head, and neck. Swelling in your feet can make it difficult to walk or stand for long periods, and you may feel pain and discomfort.
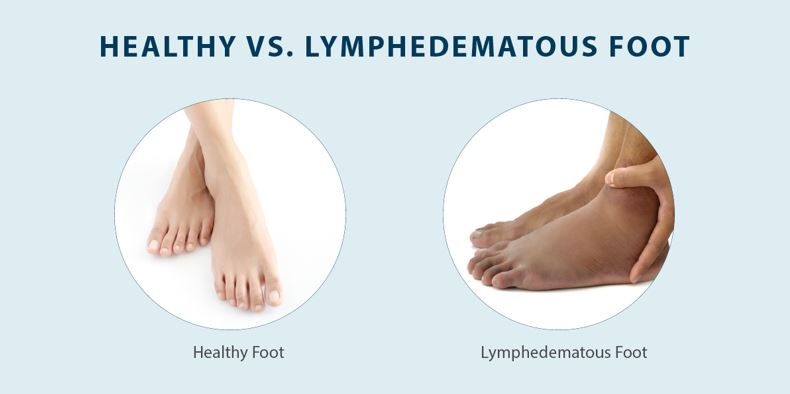
There are no exact rules as to how lymphedema in feet presents. Some individuals may have lymphedema in both feet, while others may only have lymphedema in one foot. Additionally, swelling might only affect the feet, while others may experience swelling in both their legs and feet. There are also different degrees of swelling, and measuring edema and assessing pitting edema, as well as assessing the skin, can help you and your specialist understand the stage and severity of your lymphedema.
Lymphedema in feet can be either primary or secondary. While the symptoms you experience with primary vs. secondary lymphedema in feet are similar, the treatment can vary. This is another reason why it’s crucial to visit your doctor to determine the root cause of your swelling, as lymphedema can be confused with other medical conditions. With a professional diagnosis, you can consult an expert to ensure you receive the right form of treatment.
Recognizing the symptoms of lymphedema in feet is a key part of treatment. The earlier you recognize swelling and other symptoms, the sooner you can start getting relief and prevent the progression of your condition. Below are some of the potential symptoms of lymphedema in feet:

Getting a diagnosis is a crucial part of treatment for lymphedema in feet. Diagnosing lymphedema in feet starts with a review of your medical history and a physical exam. Your doctor will look for swelling in your feet and rule out any serious medical conditions by checking you for other symptoms. This physical exam may also include a look at your medical history — especially if you’ve had cancer or cancer treatment, congestive heart failure, or other underlying health conditions.
If your doctor determines you have lymphedema, they may use additional tests such as an MRI or lymphoscintigraphy. A lymphoscintigraphy involves injecting a radioactive dye into your veins to see how fluid moves throughout your lymphatic system.5 Ultrasound may also be used to rule out lipedema, which is a buildup of fat that causes swelling. Following your doctor’s diagnosis of lymphedema, they may recommend you to a certified lymphedema therapist (CLT). The certified lymphedema specialist may give you more detailed information about your lymphedema diagnosis and treatments to help control your symptoms.
There is no cure for lymphedema, so treatment for lymphedema in feet is focused on reducing swelling and preventing complications. While you can’t cure lymphedema, you can make it easier to live with the symptoms. Here are some of the treatment methods your lymphedema specialist may recommend:

While lymphedema most commonly affects the arms and legs, lymphedema in feet is also something to be aware of. If your feet feel swollen and heavy, you should see a doctor to get a proper diagnosis. Your doctor can refer you to a specialist so you can start taking steps to manage your lymphedema.
When it comes to managing lymphedema in feet, compression is crucial. The Flexitouch Plus System and Nimbl System from Tactile Medical use pneumatic compression to reduce swelling and relieve lymphedema symptoms. Contact us to learn more about how our solutions can help you get relief from lymphedema.
References
1. FOXC2 disease-mutations identified in lymphedema-distichiasis patients cause both loss and gain of protein function. National Library of Medicine. Accessed September 11, 2023
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342337/
2. Nitti, Matthew, et al. Definition, Incidence and Pathophysiology of Lymphedema. Principles and Practice of Lymphedema Surgery. 2015. Accessed September 11, 2023. https://www.sciencedirect.com/topics/medicine-and-dentistry/lymphedema-tarda
3. Gordon K, Mortimer PS, van Zanten M, Jeffery S, Ostergaard P, Mansour S. The St George’s Classification Algorithm of Primary Lymphatic Anomalies. Lymphat Res Biol. 2021 Feb;19(1):25-30. https://pubmed.ncbi.nlm.nih.gov/33395557/
4. Domaszewska-Szostek A, Zaleska M, Olszewski WL. Hyperkeratosis in human lower limb lymphedema: the effect of stagnant tissue fluid/lymph. J Eur Acad Dermatol Venereol. 2016. Accessed September 11, 2023. https://pubmed.ncbi.nlm.nih.gov/26869365/
5. Ultrasound Elastography Use in Lower Extremity Lymphedema: A Systematic Review of the Literature. National Library of Medicine. Accessed September 11, 2023
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6820675/
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More
Stage three lymphedema is the most advanced stage of this chronic condition. In this stage, the affected body part might display one or more symptoms, such as significant swelling, alterations in the skin, or recurring episodes of infection. While this stage can be challenging to manage, understanding your condition and...
Read More
When the lymphatic system becomes compromised, fluid buildup can lead to stage 1 lymphedema, a condition marked by mild but noticeable swelling in affected areas. This initial stage is a crucial window for intervention, as proper treatment can prevent progression to more severe stages. Knowing the signs, causes, and treatment...
Read More
Living with stage 2 lymphedema brings unique challenges, but understanding your condition is the first step toward effectively managing it. While this stage marks a point where the condition becomes irreversible, there are many ways to maintain your quality of life and prevent symptoms from progressing. Keep reading to explore...
Read More
Call us at 1.800.575.1900