Lymphedema and Weight Loss
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More

Living with lymphedema requires you to follow a treatment plan to manage your symptoms and reduce the risk of complications. Taking a comprehensive approach to managing lymphedema can help you reduce swelling and avoid complications such as infection and loss of range of motion. You may be wondering who treats lymphedema and how you can get started on a treatment plan. If you’re not taking steps to manage your lymphedema symptoms, here’s what you need to know about seeing a professional and starting a lymphedema treatment plan.
What Is Lymphedema?
Who Treats Lymphedema?
How Is Lymphedema Treated?
Key Takeaways: Who Treats Lymphedema?
Lymphedema is a medical condition that causes swelling as a result of lymphatic dysfunction. The lymphatic system carries fluid through lymph vessels and nodes, and that fluid eventually drains into the bloodstream. Lymphedema occurs when there’s a blockage or damage to the lymphatic vessels that causes the fluid to build up in that region of your body. While lymphedema most commonly affects the arms and legs, it can affect any part of your body, including the head, neck, groin, abdomen, and feet.
There are two types of lymphedema: primary and secondary. Primary lymphedema is caused by a hereditary lymphatic disorder and may be present at birth — although it can also develop later in life. Secondary lymphedema is caused by an acute injury that damages the lymphatic system. Primary lymphedema is rarer than secondary lymphedema, affecting about 1 in 100,000 people. Secondary lymphedema is more common, affecting about 1 in 1,000 Americans.1 Secondary lymphedema is often caused by acute trauma, cancer, cancer treatment, blood clots, infection, or chronic venous insufficiency (CVI).
You should also be mindful of the risk factors that may increase your likelihood of developing lymphedema. People who have rheumatoid or psoriatic arthritis are at higher risk for lymphedema, as well as people of old age. Lymphedema is also more common in people who are overweight or obese, so managing your weight is a key part of lowering your risk of lymphedema.
Swelling is the most common symptom of lymphedema, but there are other symptoms you should be aware of. Many people with lymphedema have pitting, which is when pressing on the swollen area leaves an indentation in the skin. As swelling progresses, it can cause pain and heaviness in the affected limbs, make clothes and jewelry feel tighter, and lead to decreased mobility. Complications of lymphedema include an increased risk of infection, blisters, and changes in skin texture.
If you have lymphedema, following a treatment plan can help you manage your symptoms and keep your swelling under control. With proper treatment, you can reduce the risk of lymphedema from progressing and causing complications. So, what kind of healthcare provider treats lymphedema? Here are some of the most common choices for lymphedema patients.
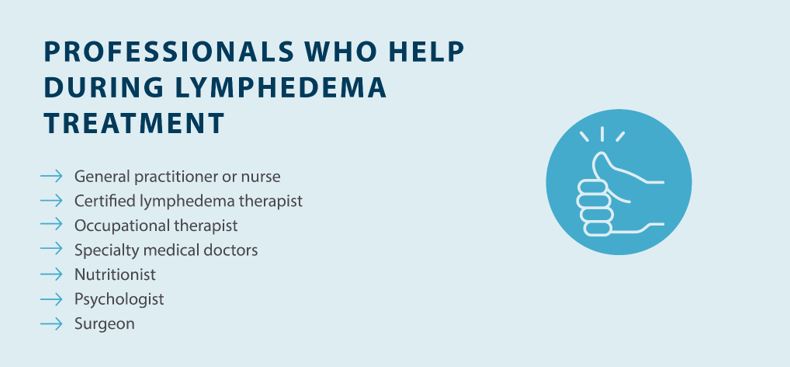
General Practitioner or Nurse
A general practitioner or nurse might be one of the first healthcare professionals you visit when you’re looking to understand your chronic swelling. There can be different causes of swelling that affect different parts of the body and a general practitioner or nurse can provide a first assessment of your symptoms to then refer you to a specialist.
Diagnosing lymphedema starts with ruling out any other potential causes of swelling. Several serious medical conditions share similar symptoms of lymphedema, and those conditions require different treatment. Your doctor may also use a lymphoscintigraphy to diagnose lymphedema. During a lymphoscintigraphy, a small amount of dye is injected into your veins to show how fluid flows through your lymphatic system. An MRI or CT scan can be used to pinpoint the swelling, and an ultrasound may be used to identify blockages in your lymphatic system.
Once you get a proper diagnosis, you can start focusing on lymphedema treatment.
Certified Lymphedema Therapist
A certified lymphedema therapist (CLT) has special training and qualifications for treating lymphedema. CLTs can come from various disciplines, such as occupational therapy, physical therapy, massage therapy, and lymphedema therapy, as all of these types of therapists require specialized training to treat lymphedema.
Your CLT can help you create a comprehensive treatment plan to reduce swelling, reduce the risk of complications, and mitigate the risk of your lymphedema progressing. Lymphedema therapists use complete decongestive therapy, which includes manual lymphatic drainage and compression, to help you manage your symptoms.
Working with an occupational therapist can be a key part of managing lymphedema. Occupational therapists offer patient-focused treatment that helps with everyday activities that are essential in life. An occupational therapist may work with your lymphedema specialist to perform a lymphatic drainage massage. Occupational therapists can also help you improve your range of motion if it’s been affected by swelling.
Of the doctors who treat lymphedema, certified lymphedema specialists are one of your most valuable resources. Specialists typically have to complete a 135-hour course in complete decongestive therapy (CDT) to become certified to ensure they have extensive knowledge and experience in treating patients.2
Medical Doctor
Depending on the cause of your lymphedema, a medical doctor may play an integral role in your diagnosis and treatment plan. Lymphedema in cancer patients is often addressed with the help of an oncologist, while lymphedema caused by CVI and other vascular diseases requires the help of a vascular specialist. Generally, patients will start with their medical doctor before being seen by a Certified Lymphedema Therapist, who implements their comprehensive treatment plan.
Medical doctors can prescribe medications and other treatments to help you get the treatment you need.
Nutritionist
Diet is an essential part of treating and managing lymphedema, and that’s where a nutritionist can help. Eating healthy and exercising can help you manage your weight and prevent lymphedema complications, but exercise alone isn’t always enough. A nutritionist or dietitian can help educate you about nutrition and make dietary changes to help you lose weight.
Your nutritionist can also help you switch to a lymphedema-friendly diet, which includes lowering your salt intake, avoiding beverages that contain caffeine or alcohol, and focusing on foods that reduce inflammation. Proper nutrition is one of many key parts that make up an effective lymphedema treatment plan.
Psychologist
Lymphedema can take a toll both physically and mentally, and your mental health is vital. Swelling and other symptoms can make it difficult to do the activities you enjoy, and changes in appearance can affect your confidence. The cost of treating lymphedema can cause financial strain that makes it difficult to focus on other aspects of life.
Working with a psychologist is a helpful way to deal with the mental health side of lymphedema. A psychologist can help you develop coping strategies and provide support that makes it easier to live with lymphedema.
Surgeon
In some lymphedema cases, surgical intervention may be options for lymphedema patients. A surgeon can perform a lymphovenous bypass or a lymph node transfer to provide relief from swelling caused by lymphedema.3 Surgery may not be a viable option for some patients due to insurance, cost, or other medical barriers, so you should talk to a doctor or specialist before considering these procedures.
Finding a surgeon who specializes in lymphedema surgery is key. Your lymphedema specialist may be able to refer you to a specialist who can perform your surgery.
There isn’t a cure for lymphedema, so your specialist will focus on treatment methods that reduce swelling and manage symptoms. Keeping up with your lymphedema treatment plan can help reduce the risk of complications such as infection. Here are some of the most essential lymphedema treatment methods:

Managing lymphedema is a lengthy process that involves a comprehensive treatment approach, so it’s important to have a network of medical professionals on your side. Your lymphedema specialist can help you create a treatment plan and find a medical doctor who treats lymphedema.
Compression devices like the Flexitouch Plus System and Nimbl System from Tactile Medical play a key role in lymphedema management for many people. These systems use pneumatic compression to reduce swelling and relieve symptoms. If you’re looking for at-home lymphedema relief, ask your lymphedema specialist about Tactile Medical’s solutions or contact us to learn more.
References
1. Sleigh BC, Manna B. Lymphedema. [Updated 2023 Apr 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537239/
2. Lymphology Association of North America. LANA Eligibility Requirements. https://www.clt-lana.org/get-certified
3. Johns Hopkins Medicine. Lymphedema: What Are Your Surgical Options? https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/lymphedema-what-are-your-surgical-options
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More
Stage three lymphedema is the most advanced stage of this chronic condition. In this stage, the affected body part might display one or more symptoms, such as significant swelling, alterations in the skin, or recurring episodes of infection. While this stage can be challenging to manage, understanding your condition and...
Read More
When the lymphatic system becomes compromised, fluid buildup can lead to stage 1 lymphedema, a condition marked by mild but noticeable swelling in affected areas. This initial stage is a crucial window for intervention, as proper treatment can prevent progression to more severe stages. Knowing the signs, causes, and treatment...
Read More
Living with stage 2 lymphedema brings unique challenges, but understanding your condition is the first step toward effectively managing it. While this stage marks a point where the condition becomes irreversible, there are many ways to maintain your quality of life and prevent symptoms from progressing. Keep reading to explore...
Read More
Call us at 1.800.575.1900