What is a Lymphatic Disorder?
What Is a Lymphatic Disorder?
A lymphatic disorder describes a disease that affects the body’s lymphatic system. Lymphatic disorders can range from mild to severe, depending on the cause and extent of the disease. Yet even in mild cases, problems with the body’s lymphatic system can have a significant impact on a patient’s quality of life and their day-to-day routine.
In this article, we provide an in-depth explanation of what lymphatic disorders are and who is at risk of developing them. We also describe how lymphatic disorders can be diagnosed and treated. Read on to learn more about what the lymphatic system is and how lymphatic disorders can have an impact on one’s health.
What Is the Lymphatic System?
What Are Lymphatic System Diseases and Disorders?
Who Is At Risk of Lymphatic Disorders?
How Are Lymphatic Disorders Diagnosed?
How Do You Treat Lymphatic Disorders?
Key Takeaways: Lymphatic Disorders
What Is the Lymphatic System?
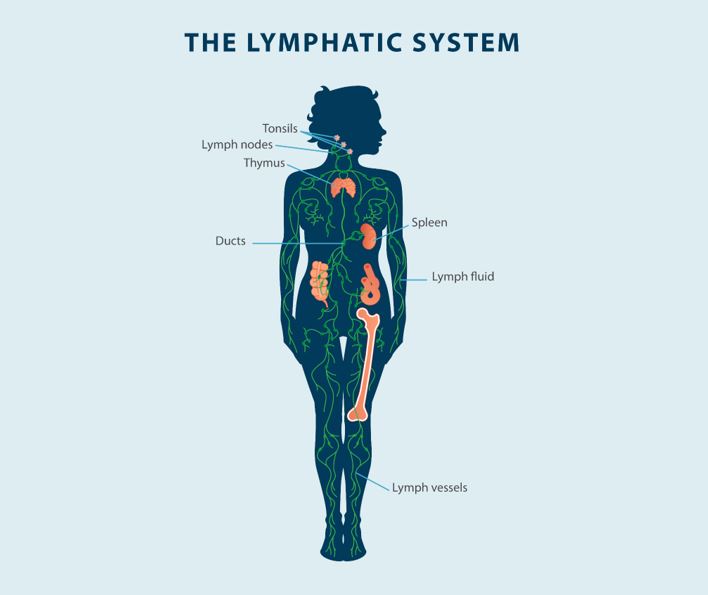
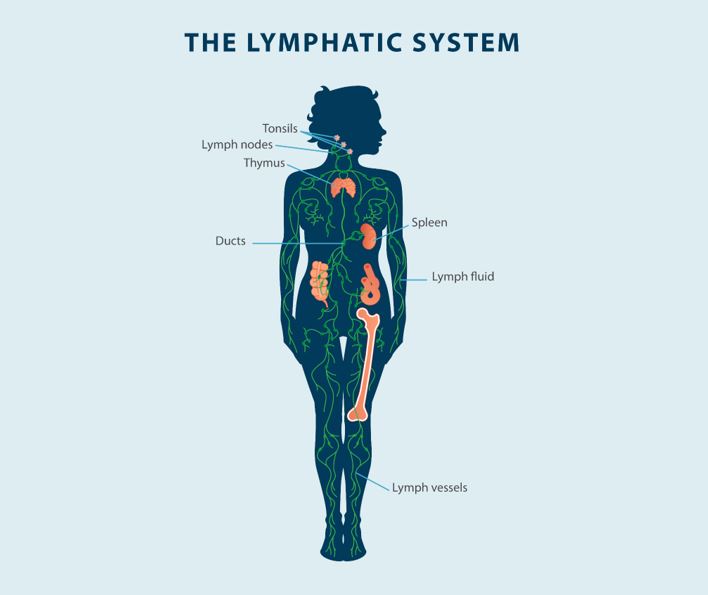
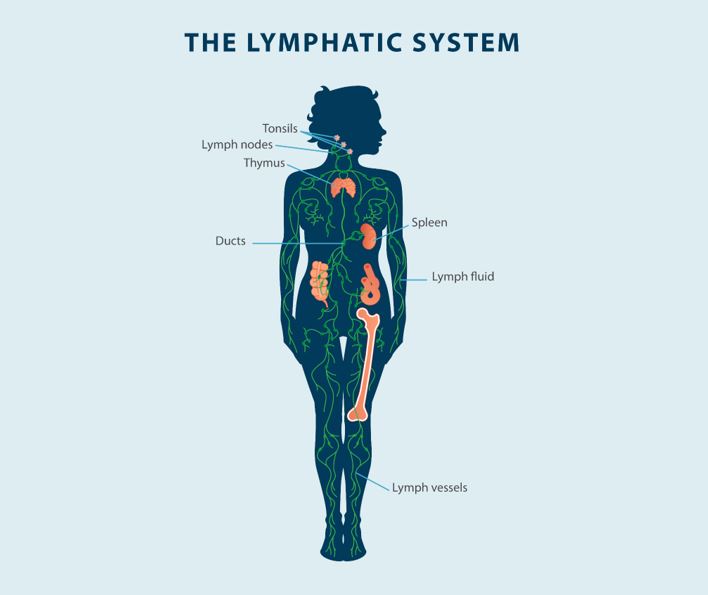
Your body circulates blood and plasma throughout the body via your blood vessels. These vessels allow your body to provide essential nutrients to cells and tissues and extract certain waste products. While most of these fluids are recirculated in your body through your blood vessels and veins, some fluids exit the blood vessels and leak into your body’s tissues. This is where the lymphatic system comes into play.
The lymphatic system is made of lymph nodes, vessels, and fluid. It is a part of your body’s immune system and is responsible for maintaining fluid levels in your body by absorbing excess fluids and leakage. By collecting excess fluids from your tissues and returning it to the bloodstream, your lymphatic system can help fight infection, manage the body’s fluid levels, and prevent the spread of cancerous cells. Lymphatic disorders, such as lymphedema, can lead to fluid buildup, swelling, and skin changes that cause discomfort and pain in a patient.
While lymphedema is the most common of all lymphatic system diseases, it is not the only one. Lymphatic disorders can present a variety of different symptoms and impact patients in different ways. Issues affecting the lymphatic system should be addressed as soon as possible to effectively manage symptoms and improve the patient’s quality of life.
The lymphatic system serves several different functions and is made up of many parts. Below, we go into more detail about the different parts of the lymphatic system and explain what role each part plays in a healthy, functioning lymphatic system.
- Lymph fluid: Lymph fluid is a clear to white fluid that travels through your body’s lymphatic system. This fluid mainly consists of a particular type of white blood cell called lymphocytes, as well as proteins, water, fat, and cellular debris. If lymph fluid is not properly drained—as in the case with patients who suffer from lymphedema—swelling can occur as the fluid builds up in the body tissues.
- Lymph vessels: Lymph vessels are the channel that carries lymph fluid throughout your lymphatic system. Lymph vessels are spread across the body and help to gather and propel lymph fluid before and after it passes through the lymph nodes.
- Lymph nodes: Lymph nodes are small clusters of tissue containing white blood cells. Your lymph nodes filter the lymph fluid as it passes through the lymph vessels, extracting bacteria and waste that may otherwise prove harmful. Lymph nodes can be found across your body and can typically be felt in your neck, armpits, abdomen, and chest.1
- Spleen: Your spleen is located just above and to the left of your stomach. The primary functions of the spleen are to filter blood and produce white blood cells, which play a key role in your body’s immune system and help to fight off infections.2
- Thymus: The thymus gland is responsible for producing and managing a special class of white blood cells called T-cells or T-lymphocytes. Mature T-cells integrate into your bloodstream and travel throughout the lymphatic system, helping to bolster your immune system and prevent infections. The thymus is primarily important during childhood development, as the gland “trains” the T-cells that will later enter your bloodstream. In adults, the thymus can typically be removed without having any significant effects on one’s health or quality of life.3
- Ducts: Lymphatic ducts are large vessels that make it possible for lymph fluid to enter your blood vessels. Allowing lymph fluid to exit the body tissues and flow into the bloodstream can help prevent infection and disease. The two primary ducts in your lymphatic system are known as the right lymphatic duct and the thoracic duct.
- Tonsils: Tonsils are lymph tissue that are positioned at the back of your mouth and around your throat. Your tonsils can help to fight off bacteria and viruses that may penetrate your body via the nose or mouth.
What Are Lymphatic System Diseases and Disorders?
Lymphatic system disorders refer to disruptions and problems that impact your body’s lymphatic system. There are several types of lymphatic system diseases and disorders, with lymphedema being the most prominent lymphatic condition. In the sections below, we cover a few of the most common lymphatic disorders so that you can familiarize yourself with what they are, how they affect you, and what causes them.
Lymphedema
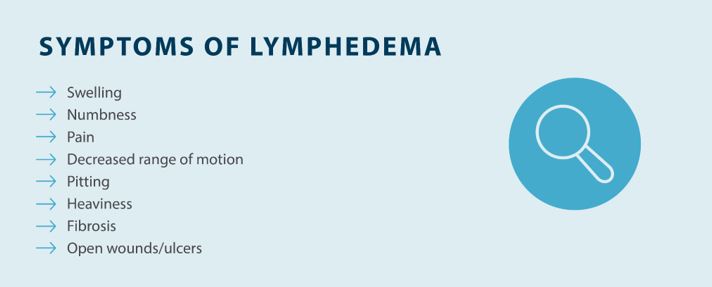
Lymphedema is a lymphatic disorder characterized by the buildup of lymph fluid in body tissues. With lymphedema, the body is unable to properly drain the lymph fluid and return it to the bloodstream, often due to an issue with one’s lymph nodes, vessels, trunks, or ducts. The fluid buildup that occurs as a result of lymphedema can lead to a number of symptoms, such as:
- Swelling or edema (especially in the arms or legs)
- A sensation of heaviness or tightness in the skin
- Numbness
- Limited range of movement
- Aching, discomfort, or pain in the affected area(s)
- Pitting of the skin
- Fibrosis
- Open wounds or ulcers
Lymphedema may occur when something disrupts, irritates, or damages the lymphatic system, impeding its ability to properly drain lymph fluid. Some of the common causes of lymphedema include:
- Undergoing cancer surgery
- Radiation therapy
- Venous disease
- Physical trauma
- Infections
- Obesity
- Diseases that impact blood flow
Keep in mind that there are two types of lymphedema: primary lymphedema and secondary lymphedema. Primary lymphedema is a condition that can be inherited or caused by spontaneous genetic mutation and present at birth or later in life, while secondary lymphedema can come about later in life due to trauma that impacts the lymphatic system. While primary lymphedema is rare, secondary lymphedema is more common, affecting approximately 1 in 1,000 Americans.4
Infections
Infections can have a negative impact on your lymphatic system by causing damage and disrupting normal functioning. In general, there are two classes of infections that impact the lymphatic system. Lymph node infections (lymphadenitis) and lymph vessel infections (lymphangitis) can disrupt your lymphatic system by targeting key elements that keep it functioning properly.5
Lymphadenitis and lymphangitis can arise from affected tissue and may affect several parts of the body, with the latter most commonly impacting the upper and lower extremities. These infections can be caused by allergies, cancer, bug bites, or infections that affect nearby tissue and spread to the lymphatic system.
In addition to lymphadenitis and lymphangitis, another infection that can affect those with lymphatic disorders, primarily lymphedema, is cellulitis. Cellulitis is a bacterial infection that affects the deep layers of skin, most commonly in the arms or legs, but can be present in any area of the body. When there is a cut or break in the skin, bacteria can enter, leading to cellulitis that can result in pain, swelling, tenderness, and fever, among other symptoms.
For patients living with lymphedema or similar lymphatic disorders, swelling can cause breaks in the skin, edema blisters, or ulcers that are prone to bacterial infections. Skin hygiene is essential when it comes to preventing infections and the progression of symptoms associated with lymphedema and other lymphatic system disorders.
Lymphoma
Lymphoma is cancer that affects the lymphatic system. There are many types of lymphoma, but the two most common types are Hodgkin’s lymphoma and Non-Hodgkin’s lymphoma. Lymphoma may affect one or more parts of your lymphatic system, and since the cancer impacts your immune system, you may be more vulnerable to infections.6
Chemotherapy and radiation therapy are often used to treat lymphoma. While these treatments can effectively push the disease into remission, they can also lead to a separate lymphatic disorder in lymphedema. Cancer, cancer surgery, and radiation therapy are all leading causes of secondary lymphedema, which is why it’s important to talk with your doctor to talk about your cancer treatment options and potential risks and rewards.
Lymphadenopathy
Lymphadenopathy is a lymphatic condition characterized by swollen or enlarged lymph nodes. Swollen lymph nodes may appear noticeably larger than usual and feel tender to the touch. In most cases, lymphadenopathy is caused by an upper respiratory infection or common illness, but generalized swollen lymph nodes—in other words, lymph node swelling in multiple parts of your body—can also indicate a more serious health condition.7
Who Is At Risk of Lymphatic Disorders?
Different people may prove more susceptible to different lymphatic disorders. Your risk of developing a lymphatic disorder depends on a multitude of factors. Things such as your age, genetics, or the presence of any preexisting health conditions can influence your likelihood of developing a lymphatic disorder.
While the risk of developing a lymphatic disorder typically varies from person to person, there are some common factors that can put you at risk for lymphatic system diseases. For instance, the following factors may elevate the likelihood of developing a lymphatic disorder:8
- Congenital heart disease
- Vascular disease
- Cancer surgery or radiation treatment
- Obesity
- Traumatic injuries
- Lymphatic obstruction
- Congenital lymphatic disorder
- Lymphatic malformations
How Are Lymphatic Disorders Diagnosed?
Just as risk factors must consider the particular lymphatic disorder and individual, the diagnostic process must also consider several unique factors. Physicians will likely take a number of factors into account as they undertake a diagnosis of a lymphatic system disease, such as a patient’s family history and personal medical history.
Once a physician suspects that a patient may have a lymphatic disorder, they can conduct tests to yield further information and come to a definitive diagnosis. Thus, in diagnosing a lymphatic disorder, the following tests or methods may be employed:8
- Physical examination: The diagnostic process for any lymphatic disorder will likely begin with a physical examination. Your physician may look for swelling and feel your lymph nodes to determine whether or not they are enlarged. A thorough history and physical exam is typically adequate to diagnose lymphedema.
- Ultrasound: An ultrasound is an imaging test and, in order to diagnose a lymphatic disorder, your doctor may conduct an ultrasound evaluation of the blood vessels, heart, or impacted soft tissues.
- Magnetic resonance imaging (MRI): Your doctor may order an MRI imaging test in order to better understand affected areas and look for signs of lymphatic disorders.
How Do You Treat Lymphatic Disorders?
Treatment plans for lymphatic system diseases and disorders will depend on the particular type of lymphatic disorder. A treatment plan may also be influenced by the severity or progression of a particular disorder.
With that being said, there are several common treatments employed to relieve symptoms of lymphatic disorders. When it comes to the most common lymphatic disorder—lymphedema—there is no cure, but there are actions one can take to manage the condition and prevent the progression of symptoms. Lymphedema treatment methods can include:
- Compression therapy: Compression therapy is one of the most common treatments for lymphatic disorders such as lymphedema. Compression garments such as compression sleeves and socks can help encourage blood flow and improve circulation, as well as prevent the accumulation of fluid.
- Manual lymphatic drainage: Manual lymphatic drainage is a type of therapeutic massage that can help promote the flow of lymphatic fluid, thereby reducing swelling and blockage.
- Weight management: Exercising and maintaining a healthy diet can help with lymphatic disorders and your overall health.
- Pneumatic compression devices: Pneumatic compression devices can help stimulate the lymphatic system. Tactile Medical’s Flexitouch Plus system can help you reduce swelling and manage lymphedema symptoms from the comfort of your own home.
Key Takeaways: Lymphatic Disorders
Lymphatic disorders impact your lymphatic system and can lead to swelling, sensations of heaviness, discomfort, and a number of other symptoms. While not all lymphatic disorders can be cured, symptoms can be managed in order to improve quality of life and ensure comfort.
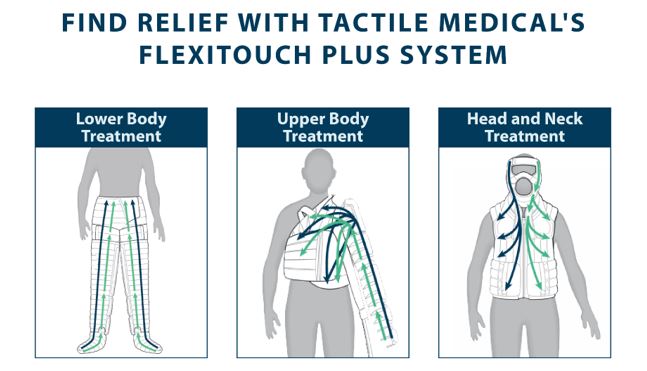
Tactile Medical offers evidence-backed lymphedema solutions that allow you to take control of your lymphatic disorder, whether it affects your upper body, your lower body, or your head and neck. Learn more about what causes lymphedema and treatment options by reading our lymphedema guide.
1. National Cancer Institute. Lymph Nodes. Cancer.gov. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/lymph-node
2. Children’s Hospital of Pittsburg. What Does the Spleen Do? https://www.chp.edu/our-services/transplant/liver/education/organs/spleen-information
3. Thapa P, Farber DL. The Role of the Thymus in the Immune Response. Thorac Surg Clin. 2019 May;29(2):123-131. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6446584/
4. Sleigh BC, Manna B. Lymphedema. [Updated 2022 Sep 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. https://www.ncbi.nlm.nih.gov/books/NBK537239/
5. Christoff J, Hebert CL, Pitrak D. Lymphatic Infections. In: Dieter RS, Dieter RA, Jr., Dieter RA, III. eds. Venous and Lymphatic Diseases. McGraw Hill; 2011. https://accesscardiology.mhmedical.com/content.aspx?bookid=1782§ionid=121400489
6. Siteman Cancer Center. Types of Lymphoma. Washington University in St. Louis School of Medicine. https://siteman.wustl.edu/treatment/cancer-types/lymphoma/types-of-lymphoma/
7. Maini R, Nagalli S. Lymphadenopathy. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. https://www.ncbi.nlm.nih.gov/books/NBK558918/
8. Nationwide Children’s Hospital. Lymphatic Disorders. https://www.nationwidechildrens.org/conditions/lymphatic-disorders