Lymphedema and Weight Loss
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More

Several medical conditions and disorders can cause lymphedema, and symptoms can start at any age. Different types of lymphedema may present different symptoms, so getting a proper diagnosis is a vital part of managing lymphedema. Your doctor can distinguish between lymphedema tarda, lymphedema praecox, and other types of lymphedema. If you recently developed lymphedema in your adult life, here’s what you need to know about lymphedema tarda.
What Is Lymphedema Tarda?
What Is the Difference Between Lymphedema Praecox and Lymphedema Tarda?
What Causes Lymphedema Tarda?
What Are the Symptoms of Lymphedema Tarda?
How Is Lymphedema Tarda Diagnosed?
How Do You Treat Lymphedema Tarda?
Wrapping Up: Lymphedema Tarda
Lymphedema tarda is a type of hereditary lymphedema that’s characterized by the age of onset. Hereditary lymphedema — a type of primary lymphedema — can be present at birth, during childhood, or during adulthood. Lymphedema tarda is a form of primary lymphedema that develops after the age of 35.1
Unlike secondary lymphedema, lymphedema tarda is caused by a genetic lymphatic disorder. Getting a diagnosis is important because it helps your doctor or specialist understand how to treat your lymphedema appropriately to better manage your symptoms and decrease the risk of progression.
Primary lymphedema is due to a genetic mutation that causes malformation of the lymphatics in the embryo. There are different types of lymphedema that develop at different ages.
Type I lymphedema is also known as congenital lymphedema, and it occurs between birth and two years old. Even though the lymphatic dysfunction that causes hereditary lymphedema may be present at birth, swelling doesn’t always start at an early age. In rare cases, lymphedema swelling may be present at birth or shortly after.1
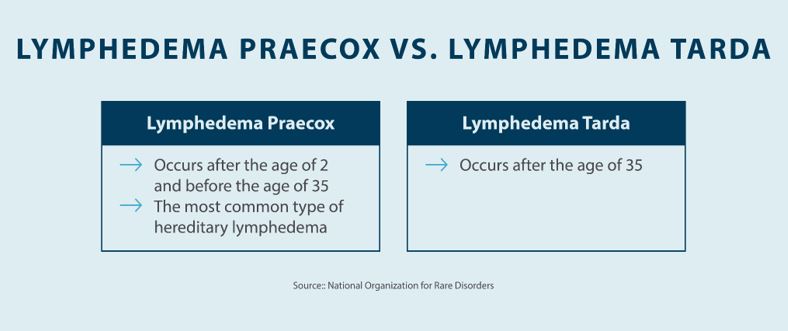
Type II lymphedema, or lymphedema praecox, occurs between 2 and 35 years old. While the lymphatic system issues are present at birth, signs of lymphedema do not present themselves until a later age. Swelling caused by lymphedema praecox generally starts to present around the age of puberty, although that can vary. The severity of lymphedema praecox symptoms can also vary.1
Lymphedema tarda is also known as type III lymphedema, which describes hereditary lymphedema that occurs after the age of 35. While research is minimal, it suggests that lymphedema tarda is caused by a genetic mutation in the FOXC2 gene.1
Determining the exact cause of lymphedema tarda can be difficult, but research suggests it’s a hereditary condition that is passed on through genetics.
Although there are no exact known lymphedema tarda causes, the condition has been associated with a mutation of the FOXC2 gene.2 This gene is responsible for the development of the valves in your veins and lymphatic system.
Recognizing symptoms is a crucial step in getting proper lymphedema tarda treatment. In this section, we’ll talk about some of the common lymphedema tarda symptoms and how they typically present. Keep in mind that you may not experience every symptom on the list — it depends on the severity of your condition.
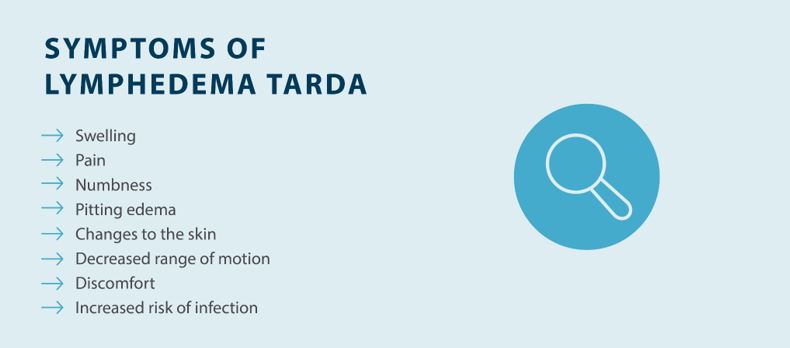
If you’re experiencing lymphedema tarda symptoms, getting a diagnosis is a crucial first step in managing lymphedema. Your doctor can help you rule out other potential medical conditions and create a lymphedema tarda treatment plan based on your diagnosis.
Diagnosing lymphedema tarda starts with a thorough exam to rule out the potential for underlying health conditions. Your symptoms could be caused by conditions like deep vein thrombosis (DVT) or congestive heart failure. Chronic venous insufficiency (CVI) can also lead to fluid imbalances, which over time, may cause lymphedema. Your doctor will also rule out secondary lymphedema, which can be caused by cancer surgery or cancer treatments, chronic venous disease, injuries, or infections.
Once your doctor has ruled out other medical conditions, they’ll use a variety of tests and techniques to diagnose you. A lymphoscintigraphy can be used to see how fluid flows throughout your lymphatic system, and MRI and ultrasounds can help your doctor pinpoint lymphatic system blockages.
Your healthcare provider may refer you to a certified lymphedema therapist for specialized treatment. Using your medical history, tests, and the age of onset, a specialist can diagnose, classify, and treat your lymphedema.
Because lymphedema is a chronic condition, lymphedema tarda treatment is focused on reducing and managing swelling to prevent complications and keep your lymphedema from progressing. Basic treatment methods, including compression, can usually control swelling. In rare cases of severe lymphedema, surgical intervention may be required. Here’s what you can expect when it comes to lymphedema tarda treatment:

Lymphedema tarda can be an unexpected development in people, as it typically occurs after the age of 35. Getting a proper diagnosis and taking steps to manage your swelling can help you keep lymphedema from progressing and lower your risk of complications. With regular treatment and management, you can live a healthier life.
Compression is an essential part of reducing and managing swelling, and Tactile Medical can help. The Flexitouch Plus System and Nimbl System are designed to provide targeted relief for swelling caused by lymphedema, helping you manage your symptoms. Ask your lymphedema specialist or contact Tactile Medical to learn more about our solutions.
References
1. Nitti, Matthew, et al. Definition, Incidence and Pathophysiology of Lymphedema. Principles and Practice of Lymphedema Surgery. 2016. Accessed September 7, 2023. https://www.sciencedirect.com/topics/medicine-and-dentistry/lymphedema-tarda
2. An approach to familial lymphedema. National Library of Medicine. Accessed September 7, 2023
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6297692/
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More
Stage three lymphedema is the most advanced stage of this chronic condition. In this stage, the affected body part might display one or more symptoms, such as significant swelling, alterations in the skin, or recurring episodes of infection. While this stage can be challenging to manage, understanding your condition and...
Read More
When the lymphatic system becomes compromised, fluid buildup can lead to stage 1 lymphedema, a condition marked by mild but noticeable swelling in affected areas. This initial stage is a crucial window for intervention, as proper treatment can prevent progression to more severe stages. Knowing the signs, causes, and treatment...
Read More
Living with stage 2 lymphedema brings unique challenges, but understanding your condition is the first step toward effectively managing it. While this stage marks a point where the condition becomes irreversible, there are many ways to maintain your quality of life and prevent symptoms from progressing. Keep reading to explore...
Read More
Call us at 1.800.575.1900