Phlebolymphedema: All you Need to Know
Phlebolymphedema Guide: What Is Phlebolymphedema?
Phlebolymphedema is a type of lymphedema that involves a combination of chronic venous insufficiency and lymphatic drainage issues. This condition leads to swelling as a result of a buildup of fluid in the body tissue. As swelling increases and persists over time, it can lead to complications ranging from pain and discomfort to ulcers and infections. In this guide, we’ll explore phlebolymphedema in depth, including symptoms, causes, treatment, and more.
What Is Lymphedema?
What Is Phlebolymphedema?
What Is the Connection Between Lymphedema and Phlebolymphedema?
Why Does Early Detection Matter?
What Are the Symptoms of Phlebolymphedema?
How Is Phlebolymphedema Diagnosed?
What Causes Phlebolymphedema?
How Do You Treat Phlebolymphedema?
How Tactile Medical Can Help
What Is Lymphedema?
Lymphedema is a type of edema caused by lymphatic dysfunction, or a problem with the lymphatic system. Your lymphatic system consists of a series of lymph vessels that carry lymph fluid. In a healthy body, lymph passes through many lymph nodes that filter out cellular debris, waste, and damaged cells. The lymph fluid continues to be processed and eventually returns to your bloodstream.
However, when there’s a blockage that causes lymph fluid to build up, it results in lymphedema. Lymphedema refers to the accumulation of fluid that results in swelling. Lymphedema can be primary or secondary, where primary lymphedema is present at birth and caused by genetics, while secondary lymphedema is caused by damage to the lymphatic system, such as an injury, cancer, or cancer treatment.
What Is Phlebolymphedema?
Whereas lymphedema is a result of lymphatic dysfunction, phlebolymphedema is a condition that’s caused by a combination of both chronic venous insufficiency (CVI) and lymphatic dysfunction.1
In a healthy person, blood is able to circulate throughout your body and return back to the heart. In patients with CVI, valves in the lower legs are unable to close completely, causing blood to flow backward. When this occurs, swelling may begin to occur in the lower legs, ankles, and feet. As CVI advances, it can result in lymphatic overload that leads to phlebolymphedema.2
What Is the Connection Between Lymphedema and Phlebolymphedema?
Patients with lymphedema experience swelling as a result of a buildup of lymph fluid. This swelling occurs because lymph fluid is unable to pass through a lymph node or vessel, which causes it to accumulate in body tissue instead. Those living with lymphedema can experience swelling and other symptoms in various parts of the body, such as the head and neck, upper body, groin, arms, abdomen, and lower body.
Phlebolymphedema is similar to lymphedema but is the result of the combination of chronic venous insufficiency and lymphatic dysfunction. As a two-system failure, a phlebolymphedema patient will experience swelling that’s caused by vascular issues leading to lymphatic dysfunction, and if clinicians fail to address both the veins and the lymphatics, then the downward spiral of symptoms will continue. It’s important to note that multiple factors are at play when it comes to the development of phlebolymphedema, which prevents the lymphatic system from draining fluids properly.
Of all the different types of lymphedema, phlebolymphedema is the most common type of lymphedema in the Western world.1
Why Does Early Detection Matter?
Lymphedema and phlebolymphedema are chronic conditions that pose symptoms like swelling, pain, decreased mobility, and discomfort. While symptoms can be mild in early stages, complications can arise if preventative measures aren’t taken early on to reduce the progression of symptoms. Early detection helps you get started on your phlebolymphedema treatment plan as soon as possible. That way, you can minimize your symptoms and prevent some of the complications that can arise, such as an increase in infections or pain.
If you’re experiencing any symptoms that you think may be related to phlebolymphedema, lipedema, or any type of edema, you should schedule an appointment with your doctor at your earliest convenience. Your doctor can diagnose your condition using a basic clinical exam and, in some cases, imaging tests. Phlebolymphedema can be diagnosed during a clinical examination, so make sure you talk to your doctor about your medical history and all the symptoms you’re experiencing.
If your doctor is having trouble with a diagnosis or doesn’t think you have phlebolymphedema, consider getting a second opinion from another doctor or specialist. Lymphedema and phlebolymphedema are still understudied, and some physicians may not have the knowledge or experience to help. Early detection is key with all forms of lymphedema, as it can help you manage your symptoms and reduce chronic swelling.
What Are the Symptoms of Phlebolymphedema?
Recognizing that you have — or may have — phlebolymphedema is one of the most important steps in treating and managing your condition. These symptoms are a sign that your swelling may be caused by a medical condition that requires treatment. If you’re experiencing any of the following phlebolymphedema symptoms, you should visit a doctor:1
- Pain: The swelling caused by any type of lymphedema can lead to pain in many cases. Pain typically occurs in the area where swelling occurs due to increased inflammation. Pain caused by phlebolymphedema typically subsides when you reduce swelling, so taking measures to treat swelling is key.
- Venous leg ulcers: Patients with phlebolymphedema or chronic venous insufficiency are susceptible to venous leg ulcers, which are slow-to-heal wounds that are caused by damaged valves in the veins, resulting in a buildup of excess pressure and fluid. These ulcers are large sores that appear on the affected limbs as a result of venous insufficiency and are susceptible to infection, which can further worsen phlebolymphedema symptoms.
- Swelling: Swelling is the most common symptom of phlebolymphedema because of the lymphatic fluid and blood that’s building up in your body. Swelling can lead to a wide range of other symptoms, including pain, decreased mobility, and thickened skin.
- Trouble walking: Increased swelling from phlebolymphedema can make it difficult to walk. A combination of pain and swelling makes it challenging for phlebolymphedema patients to move around comfortably, which can have both a physical and mental impact.
- Recurring infections: Both lymphedema and chronic venous insufficiency can make people more prone to infections, so you may experience recurring infections as a result. This is because swelling can cause the skin to crack or for venous leg ulcers to appear, making it easier for bacteria to enter the tissues and lymphatic vessels. To reduce the risk of infections like cellulitis, regularly monitor your skin for any wounds or cuts on your legs and feet, as infections can lead to serious complications.
- Decrease in mobility: Swelling in the legs can lead to decreased mobility, with some patients being stuck in bed for most of the day as a result of phlebolymphedema. If your mobility is affected by your lymphedema, you should visit a doctor as soon as possible to create a treatment plan to regain your quality of life.
- Hard, thick, or discolored skin: As phlebolymphedema progresses, it may lead to changes in the color and texture of your skin. If you notice hard, thick, or discolored skin on your legs, that may be a sign of phlebolymphedema or another type of edema.
How Is Phlebolymphedema Diagnosed?
Diagnosing phlebolymphedema is a crucial first step in getting the treatment you need to live a comfortable life and avoid complications. So, what can you expect when you go to the doctor to have your phlebolymphedema diagnosed?
Doctors typically begin diagnosing phlebolymphedema with a basic clinical exam. Your doctor will ask you about the symptoms you’re experiencing and examine your legs to check for swelling, skin problems, and other signs of phlebolymphedema.
Another simple diagnostic method your doctor may use is the Kaposi-Stemmer’s sign, where they will pinch a fold of skin. Typically, a doctor will pinch a fold of skin on the top of one of your toes, but this method can be used in other areas of the body, such as the legs or arms. If the skin easily tents, it is classified as a negative result, whereas a positive Kaposi-Stemmer’s sign occurs when the skin cannot be pinched. This is because it indicates that lymph fluid is preventing the redistribution of interstitial fluids.1 However, a negative Kaposi-Stemmer sign isn’t always accurate, so further assessments may have to be done.
Your doctor might also look at your medical history to see if you have risk factors. Oftentimes, this clinical examination is enough to diagnose phlebolymphedema, but that’s not always the case.
In the event that a clinical exam isn’t enough, your doctor may also use imaging tests. These tests are more involved than a basic exam but offer accurate results. If you’re having trouble getting a diagnosis from your doctor, you can inquire about a lymphoscintigraphy or echo-Doppler test.
What Causes Phlebolymphedema?
There are several factors that can cause phlebolymphedema, and knowing the causes can help you better understand the condition. For some, phlebolymphedema occurs as a result of genetics, while others can be diagnosed with the condition due to certain types of acute trauma. Here are some of the most common causes of lymphedema and phlebolymphedema:
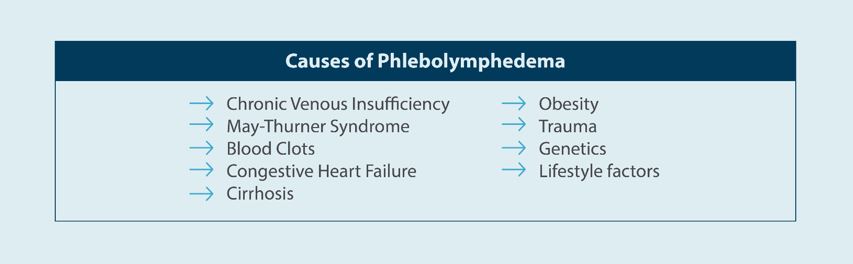
- Chronic Venous Insufficiency (CVI): Chronic venous insufficiency occurs as a result of damage to valves in your leg veins. When these valves are damaged, they have difficulty circulating blood, causing blood to pool that can result in swelling and ulcers. CVI is the leading cause of phlebolymphedema.
- May-Thurner Syndrome: May-Thurner syndrome is a medical condition that’s caused by an artery compressing a vein — specifically the right iliac artery and the left iliac vein. Complications of May-Thurner syndrome include swelling, pain, and deep vein thrombosis.3
- Deep Vein Thrombosis (DVT): DVT, more commonly known as a blood clot, is a clot that occurs in a deep vein. These clots are particularly dangerous because they can lead to a pulmonary embolism if the clot is dislodged and makes its way to the lungs.4 Blood clots can also lead to a condition called Post-Thrombotic Syndrome (PTS), which may cause chronic pain and swelling. PTS may develop in the weeks for months following a DVT.
- Congestive Heart Failure: Heart failure occurs when the muscles in your heart aren’t able to pump blood efficiently. Congestive heart failure can cause phlebolymphedema because the buildup of blood puts pressure on the veins, causing fluid to leak out of the veins and into the tissues. Over time, this may lead to swelling.5
- Cirrhosis: Cirrhosis is scarring in the liver that results from the liver trying to repair itself after it’s damaged. Repeated damage from alcohol abuse and conditions like hepatitis can eventually lead to cirrhosis, which is late-stage scarring of the liver. Cirrhosis can cause lymphatic dysfunction that leads to various forms of lymphedema.1
- Obesity: Obesity contributes to a wide range of medical conditions, including phlebolymphedema. Obese people are at an increased risk of phlebolymphedema due to excess adipose tissue (fat) placing pressure on lymphatic nodes and vessels.
- Trauma: Acute trauma to the veins or lymphatic system can lead to phlebolymphedema. This trauma may occur as a result of an injury or surgery, such as direct trauma or injury or extensive burns.
- Genetics: Some people are more likely to get phlebolymphedema as a result of their genetics. If you have a genetic predisposition to CVI or phlebolymphedema, make sure you keep an eye out for any symptoms.
- Lifestyle factors: Living a sedentary lifestyle, smoking, and sitting for extended periods of time can all increase your risk of developing phlebolymphedema.
How Do You Treat Phlebolymphedema?
There is no cure for phlebolymphedema, which means the focus of phlebolymphedema treatment is on managing symptoms and preventing its progression. Below are some of the most common phlebolymphedema treatment and management methods:
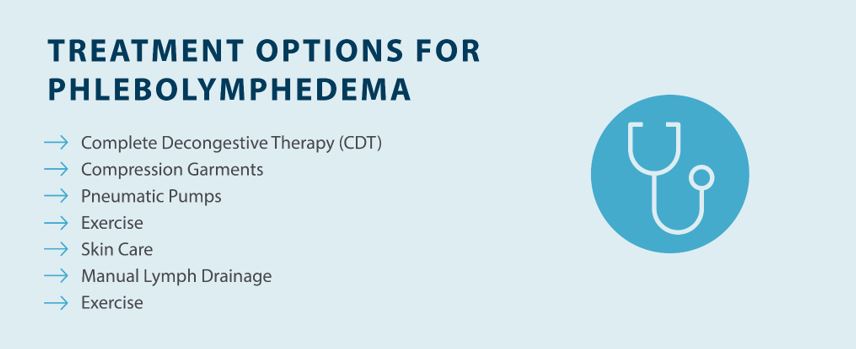
- Complete Decongestive Therapy (CDT): Complete decongestive therapy combines various techniques, including manual lymphatic drainage, exercise, compression, and skin care, to help reduce swelling and prevent complications caused by phlebolymphedema.
- Compression Garments: Compression garments can be worn to help reduce swelling, but you should always talk to your doctor before wearing medical grade compression garments.
- Pneumatic Pumps: Pneumatic pumps can help reduce swelling caused by lymphedema by applying gentle pressure and guiding fluid away from swollen areas.
- Exercise: Regular exercise encourages blood flow and helps patients manage their weight, which are important steps in treating and managing phlebolymphedema.
- Skin Care: Taking care of your skin, including moisturizing, wearing sunscreen, and keeping your skin clean, helps prevent complications such as skin ulcers and infections.
- Manual Lymph Drainage: Manual lymphatic drainage massages can be performed at home or by a specialist to help guide lymphatic fluid away from damaged parts of the lymphatic system.
How Tactile Medical Can Help
Living with phlebolymphedema can make life challenging, especially if you’re having trouble staying active as a result. If you’re diagnosed with phlebolymphedema, the best thing you can do is start a treatment plan right away to relieve symptoms and prevent complications.
If you’re dealing with swelling and pain as a result of phlebolymphedema, Tactile Medical’s solutions can help. Our pneumatic compression devices help gently guide lymph away from swollen parts of the body so you can get relief. Check out the Flexitouch Plus system by Tactile Medical to learn more today.
________________________________________
Sources:
1. Farrow W. Phlebolymphedema-a common underdiagnosed and undertreated problem in the wound care clinic. J Am Col Certif Wound Spec. 2010 Apr 22;2(1):14-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601853/
2. Ashforth, Karen. Understanding Lower Extremity Phlebolymphedema Fibrosis. Lymphatic Education & Research Network. https://lymphaticnetwork.org/news-events/understanding-lower-extremity-phlebolymphedema-fibrosis
3. Peters M, Syed RK, Katz M, Moscona J, Press C, Nijjar V, Bisharat M, Baldwin D. May-Thurner syndrome: a not so uncommon cause of a common condition. Proc (Bayl Univ Med Cent). 2012 Jul;25(3):231-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377287/
4. National Center on Birth Defects and Developmental Disabilities , Centers for Disease Control and Prevention. What is Venous Thromboembolism? 2022 Jun. https://www.cdc.gov/ncbddd/dvt/facts.html
5. Reid, Tony. Congestive Heart Failure. http://www.lymphedema.com/heart.htm