Arm Swelling: How to Reduce Swelling in Your Arm
Read More
Peripheral edema is a swelling that occurs when fluid accumulates in the tissues of your extremities. It typically affects the legs, ankles, and feet. This condition can be accompanied by mild to severe discomfort, which impacts daily activities and quality of life, making it essential to understand its causes, recognize its symptoms, and explore treatment options to manage it effectively.
Keep reading to learn everything you need to know about peripheral edema.
Peripheral edema causes swelling due to the accumulation of fluid in the tissues of your extremities, resulting in noticeable swelling that typically affects your legs, ankles, and feet, although it can also occur in your arms and hands. This condition develops when your body’s circulatory system cannot effectively move fluid back toward your heart, causing it to pool in the interstitial spaces between cells in your limbs.1
Unlike generalized swelling, which affects the entire body, peripheral edema specifically targets the extremities and often appears more pronounced in dependent areas, where gravity naturally pulls fluid downward. The fluid that accumulates can’t be adequately drained by the lymphatic vessels and nodes.
This type of edema primarily affects the periphery of your body rather than central organs or tissues. Untreated edema can worsen over time and lead to complications, making early recognition and treatment important.
Understanding what triggers peripheral edema can help you recognize risk factors and take steps to address them. Causes of peripheral edema fall into three main categories: lifestyle and temporary factors, underlying medical conditions, and medications that can contribute to fluid retention.
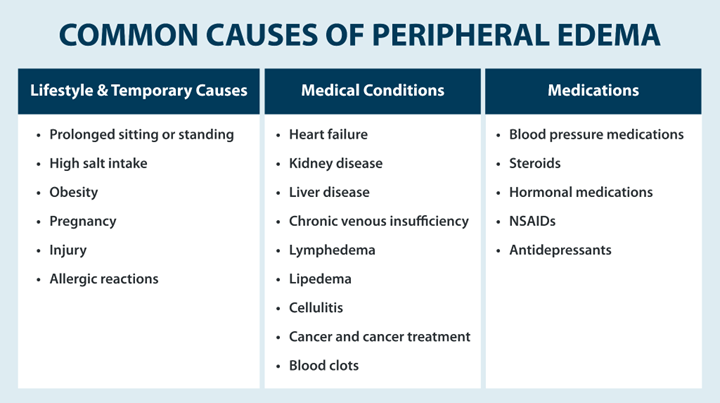
Several everyday situations and lifestyle factors can lead to peripheral edema, which often resolves once the underlying cause is addressed. These include:1
Various health conditions can disrupt your body’s ability to maintain proper fluid balance, leading to peripheral edema as a symptom.1
Certain medications can contribute to peripheral edema as a side effect by affecting fluid balance or circulation. These include:1
Recognizing the signs of peripheral edema early can help you seek appropriate treatment and prevent the condition from worsening. Peripheral edema symptoms typically develop gradually and may vary in severity.1
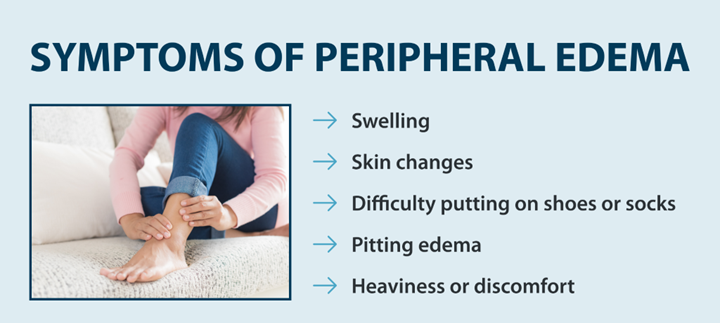
Healthcare providers often use specific techniques for measuring edema to track progression and treatment effectiveness. This may include circumferential measurements of affected limbs or standardized assessment tools to document changes over time.
Treatment for peripheral edema focuses on reducing fluid accumulation and addressing the underlying cause of the condition. Your healthcare provider may recommend complete decongestive therapy, which is a comprehensive treatment plan that combines multiple approaches. The specific strategies in your plan may vary depending on the severity of your condition and its underlying cause, but several techniques can help manage symptoms and improve your comfort.1
Early detection and proactive treatment of peripheral edema can improve your quality of life. If you’re experiencing persistent swelling in your extremities, it’s always a good idea to work with a healthcare provider who can create an effective treatment plan.
For individuals with conditions such as lymphedema or chronic venous insufficiency, doctor-prescribed pneumatic compression devices, like Tactile Medical’s Flexitouch Plus and Nimbl systems, can offer effective and convenient treatment options that help manage symptoms and improve daily comfort.
References
1. Goyal A, Singh B, Afzal M. Peripheral Edema. [Updated 2025 Apr 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554452/
Read More
Edema can affect any part of the body, but in some cases, it may only present itself in one leg. Edema in one leg is typically caused by a localized injury or lymphatic malformation that leads to swelling. Swelling in one leg can cause discomfort and affect your daily life,...
Read More
Edema can lead to several symptoms, including edema bruising. People with edema typically bruise more easily, and those bruises may be accompanied by pain. Understanding the symptoms of edema and how to manage chronic swelling can help you control your symptoms and prevent complications.
Read More
Measuring edema can help you get an accurate diagnosis. Learn how edema assessments are performed, along with treatment and other information, here.
Read More
Call us at 1.800.575.1900