Peripheral Edema
Review our guide on peripheral edema to learn about its symptoms, causes, and treatment, so you can manage your condition.
Read More
Measuring edema is a crucial step in keeping an eye on your symptoms and managing your edema. Edema assessments should be a routine part of your edema management plan, as it allows you to monitor your edema to better understand its severity and what your best treatment options are. Routine edema measurements can also help you prevent your edema from worsening over time. If you want to know more about how to measure edema and what you can do to manage your symptoms, review our guide below.
What Is Edema?
What Causes Edema?
How Is Edema Assessed?
History Assessment
Physical Assessment
How Do You Measure Edema?
Edema Measurement Chart
Can You Treat Edema?
Manage Edema Symptoms at Home With Tactile Medical
Edema is a medical condition that’s caused by a buildup of excess fluid in the body tissue. Edema can occur in any part of the body but is most common in the hands, arms, feet, ankles, and legs. This swelling can lead to various symptoms, including pain, skin that feels stretched or appears shiny, and swelling in the affected area. In some cases, you may have pitting edema, which is a type of edema characterized by dents or pits left in the skin after pressure is applied.
While edema may not present a serious risk at first, it can eventually progress to the point that it causes serious complications. For example, if acute edema is left untreated, over time, it can lead to lymphedema. If you’re diagnosed with edema, you should talk to a doctor about reducing swelling and preventing edema complications. Lifestyle changes and at-home treatment can help prevent complications and allow you to maintain your quality of life.
Understanding the causes of edema and how to perform an edema assessment are important parts of preventing its progression and managing symptoms. Edema is caused when blood vessels in your body leak fluid into the surrounding tissue, and the lymphatic system is unable to absorb this fluid effectively. Here are some of the potential causes of edema that you should keep in mind:1

A routine edema assessment can help you avoid treating edema blisters and other potential symptoms of edema. When diagnosed with edema, your doctor will perform an assessment to determine the severity of your edema. Physicians use a history assessment as well as a physical assessment to measure edema. We’ll take a closer look at how those assessments work below.
History assessments can help your physician understand when you first noticed edema symptoms and what may have caused your edema. By understanding your medical history and the onset of your edema, physicians can get a better understanding of how to treat and manage your condition. Here’s how history assessments work:1
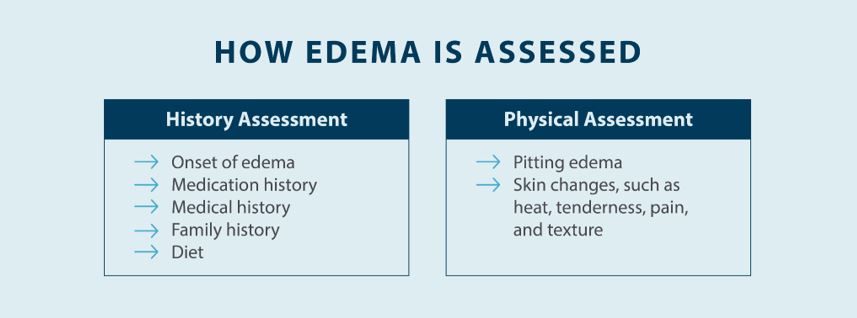
The next step is performing a physical assessment to determine the severity of the swelling. Understanding your medical history helps your physician understand how long you’ve had edema and what your best treatment options may be, but performing a physical assessment to get an edema measurement is essential. Here’s what your physician will do to physically assess your edema:1
Measuring edema is a vital part of determining the best treatment plan and taking steps to manage symptoms, such as implementing complete decongestive therapy. Your edema measurement will help determine what kind of treatment plan is right for you, and it will also help you figure out whether your edema is progressing or not. If you want to know more about how to measure edema and what the different edema measurements mean, here’s how each measurement is taken:
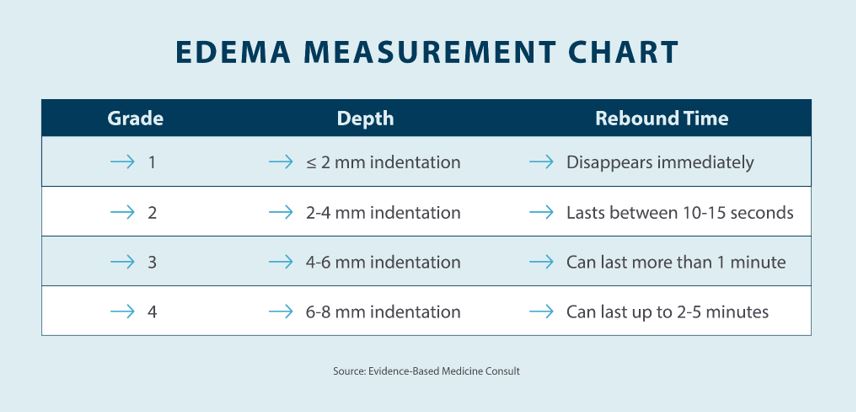
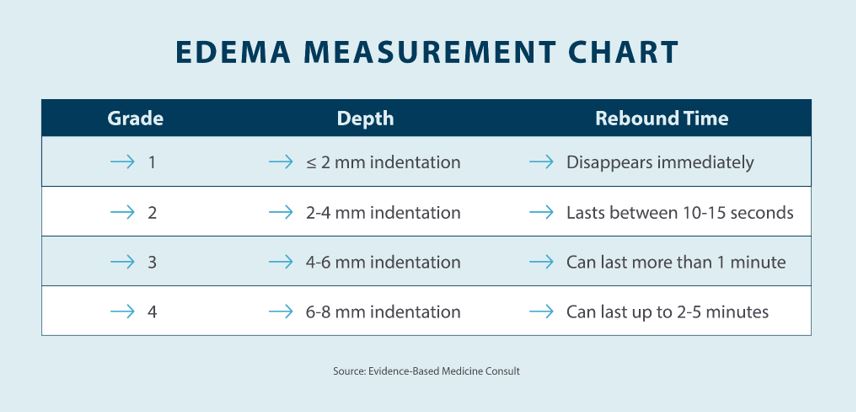
Now that you understand the basics when it comes to assessing and measuring edema, you might be wondering what those edema measurements actually mean. When you visit a doctor or specialist, you should figure out the volume and girth of your edema as well as the grade of your pitting. You can find out more about what each of these numbers means in the edema measurement chart below.3
One of the challenges of living with edema is that it’s not always easy to treat. Treatment for edema depends on the cause of your edema, which is why it’s so important to visit a professional for an edema assessment. Your physician can help you determine the cause and severity of your edema and help you create a treatment plan that works for you. Here are some of the edema treatment options your physician may recommend:
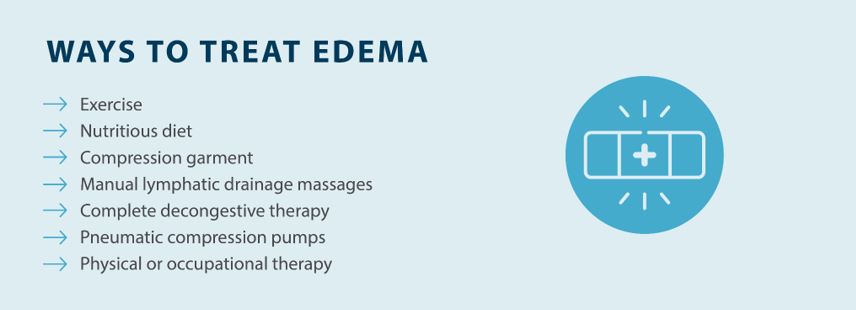
Measuring edema is a crucial part of figuring out how severe your edema is and how you should treat it. Your physician can also help you determine the potential cause of your edema with a history assessment. When it comes to getting relief from edema, Tactile Medical can help with our Flexitouch Plus System. With the Flexitouch Plus System, you get targeted relief from edema thanks to pneumatic compression, and there are devices available for your lower body, upper body, and even your head and neck. Try the Flexitouch Plus System from Tactile Medical and get the edema relief you deserve at home.
Sources:
1. Trayes KP, Studdiford JS, Pickle S, Tully AS. Edema: diagnosis and management. American Family Physician. 2013;88(2):102-10. https://www.aafp.org/pubs/afp/issues/2013/0715/p102.html
2. O’Sullivan, S.B. and Schmitz T.J. (Eds.). (2007). Physical rehabilitation: assessment and treatment (5th ed.). Philadelphia: F. A. Davis Company. p.659 https://geriatrictoolkit.missouri.edu/cv/pitting_edema.html
3. Busti, Anthony J. Pitting Edema Assessment. Evidence-Based Medicine Consult. 2016. https://www.ebmconsult.com/articles/pitting-edema-assessment
Review our guide on peripheral edema to learn about its symptoms, causes, and treatment, so you can manage your condition.
Read More
Read More
Edema can affect any part of the body, but in some cases, it may only present itself in one leg. Edema in one leg is typically caused by a localized injury or lymphatic malformation that leads to swelling. Swelling in one leg can cause discomfort and affect your daily life,...
Read More
Edema can lead to several symptoms, including edema bruising. People with edema typically bruise more easily, and those bruises may be accompanied by pain. Understanding the symptoms of edema and how to manage chronic swelling can help you control your symptoms and prevent complications.
Read More
Call us at 1.800.575.1900