Upper Body Lymphedema Solutions
Lymphedema is a chronic, progressive condition that can be measured in stages, making early intervention and daily management essential for the best outcomes. Discover our upper body lymphedema treatment solutions that help promote lymphatic circulation in the hands, arms, and chest.
Find Relief at Home with the Flexitouch Plus® or Nimbl™ systems
Explore our pneumatic compression arm pumps and upper body lymphedema solutions to find convenient relief at home. Our Flexitouch® Plus and Nimbl™ systems deliver intermittent compression to relieve upper body swelling, pain, and related lymphedema symptoms for a better quality of life. Lymphedema pumps for the arm can be worn once per day for an hour and complement compression arm sleeves and garments that can be worn throughout the day.
Flexitouch Plus provides a comfortable, effective, at-home treatment designed to help head and neck lymphedema patients get back to their lives.
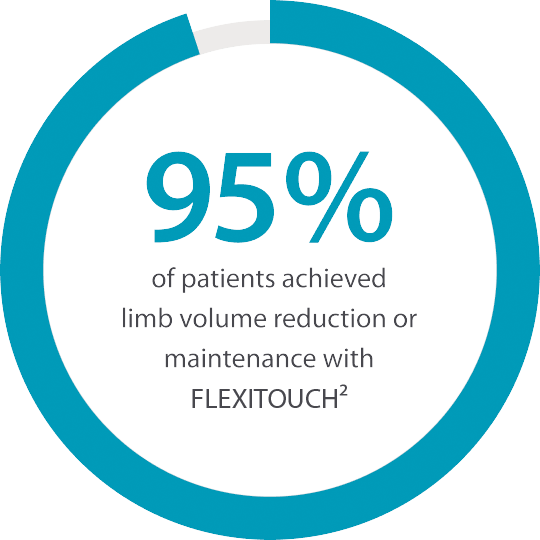
The Flexitouch Plus system is clinically proven to stimulate the lymphatic system. This advanced pneumatic compression device (lymphedema pump) gives patients a comfortable and convenient way to self-manage lymphedema.
Flexitouch Plus treatments are:
Clinically Proven: Clinical evidence shows Flexitouch is proven to work better than self-MLD, basic pumps, or standard therapy with self-care alone.
Consistent: Unlike manual lymphatic drainage (MLD), effective treatment doesn’t depend on patient technique or ability. Repeatable results and high patient satisfaction encourage ongoing use and better outcomes.
Comfortable: Garments are made of soft, comfortable fabric while the dynamic pressure feels like a soothing massage.
Convenient: Outcomes are driven by daily management; a great home tool makes all the difference.
Discover
Flexitouch® Plus
for Upper Body
Empowering patients to self-manage their upper extremity lymphedema from home for improved outcomes and a better quality of life.
Discover
Nimbl™
for Upper Body
Innovative and effective basic pneumatic compression therapy for the upper body, with a small, light, compact, and connected controller designed for an improved patient experience.
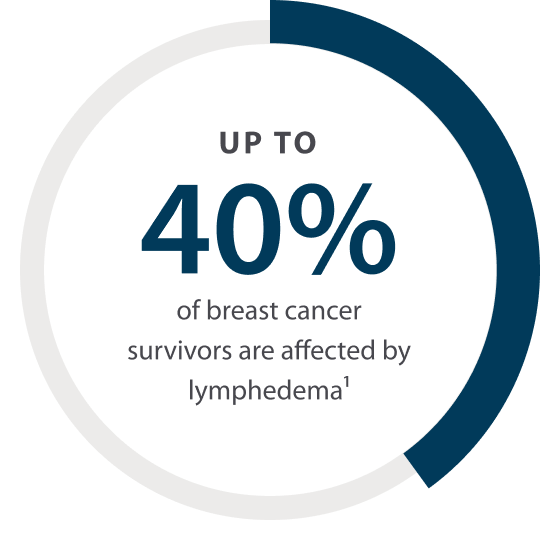
Breast cancer survivors often face another challenge: swelling that doesn’t go away, also known as lymphedema.
Even as cancer treatment has evolved, many patients still go on to develop lymphedema. Radiation, lymph node removal and taxane-based chemotherapy, combined with patient risk factors, like obesity, result in lymphedema for up to 40% of breast cancer survivors.1
Lymphedema isn’t “just swelling.” A compromised lymphatic system can also lead to skin hardening and a compromised immune function that impacts not only daily activities, but psychosocial, economic and health outcomes.
As with any chronic, progressive condition, early intervention and practical tools for daily management create the best results.
Discover Our Solutions
No matter where you may have swelling, we can help.
In many cases, the sooner you treat chronic swelling, the better for your long-term health. Explore our at-home upper body lymphedema therapy solutions, designed to treat your swelling on your own time, so you can get back to living your best life.
Upcoming webinars
Register for our upcoming live webinars or take a look at past webinars and other resources for the latest research
Need help now? We’re here for you.
Call us at 1.833.3TACTILE (1-833-382-2845)
Upper Body Lymphedema FAQs
What is upper body lymphedema?
Upper body lymphedema is a chronic and progressive condition resulting from damage or malformation of the lymphatic system that causes a buildup of fluid in the tissues in regions of the upper body, such as the hands, arms, and chest, resulting in swelling. While lymphedema can’t be cured, various treatment options exist, from using arm pumps for lymphedema to making lifestyle changes like exercise and a healthy diet, along with compression arm sleeves to promote circulation.
What are the stages of upper body lymphedema?
Lymphedema is typically described in three stages, which help guide treatment and management:
- Stage 0 Lymphedema (Minor): Impaired lymphatic function begins, but swelling may not be apparent. Symptoms are often minor, including heaviness, tingling, or tightness.
- Stage 1 Lymphedema (Mild): Swelling is soft and may return to a normal size with elevation. Skin appears normal, pitting edema may be present, and symptoms may come and go.
- Stage 2 Lymphedema (Moderate): Swelling becomes more persistent and does not resolve with elevation. More significant skin changes appear, where the skin may feel firmer, thicker, or spongy due to the development of fibrous tissue.
- Stage 3 Lymphedema (Severe): Swelling is significant and permanent, with hardening of the skin (fibrosis) and possible changes in skin texture or color.
Early detection and treatment at any stage can help prevent progression and improve quality of life.
What are the causes of upper body lymphedema?
The causes of lymphedema in the upper body can be the result of genetics, which is known as primary lymphedema, or caused by damage to the lymphatic system, known as secondary lymphedema. Secondary upper body lymphedema is more common, and lymphedema risk factors include:
- Cancer, radiation therapy, and cancer surgery: The removal of a lymph node or damage to nodes or vessels from cancer, cancer surgery, and radiation therapy, are the most common causes of upper body lymphedema.
- Infections: Infections like cellulitis can scar and inflame lymph vessels, making it more difficult for them to drain and circulate fluid properly.
- Venous diseases: Venous conditions, such as blood clots (deep vein thrombosis) or chronic venous disease, can strain the lymphatic system, causing chronic swelling.
- Trauma: Injuries from accidents or burns that damage the lymphatics can lead to upper body lymphedema, as damaged lymph nodes or vessels can have difficulty circulating lymphatic fluid from the injured area.
- Obesity: While more likely to cause lower body lymphedema, obesity can cause lymphedema in the upper body, as excess weight can compress lymph nodes and vessels, which makes it more difficult for fluid to flow, causing swelling.
What are the symptoms of upper body lymphedema?
The symptoms of lymphedema in the arms and upper body can vary from patient to patient. However, some of the common signs of upper body lymphedema:
- Swelling in the arms, chest, trunk, or abdomen that can range from mild puffiness to noticeable swelling
- Tightness and discomfort in the affected area that can make the skin, clothing, or jewelry feel tighter
- Limited range of motion, which can make it difficult to move the arms, shoulders, or hands
- Changes in skin texture where the skin becomes shiny, thick, or hard, along with discoloration and the development of rashes or blisters.
- Increased risk and occurrence of infections
How do you treat upper body lymphedema?
The treatment of upper body lymphedema involves a multifaceted approach that follows the elements of complete decongestive therapy (CDT). CDT is a noninvasive treatment program that combines in-clinic care and self-management at home. Components of CDT include manual lymphatic drainage, compression, exercise, and skin care:
- Manual lymphatic drainage (MLD): MLD is a specialized massage technique that encourages the flow of fluid throughout the body to reduce swelling. Pneumatic compression pumps for the arm, such as the Flexitouch Plus and Nimbl systems, are often recommended by doctors for at-home maintenance of swelling and related lymphedema symptoms.
- Compression: Compression garment (sleeves) for lymphedema help improve circulation to reduce swelling and pain.
- Exercise: Upper body lymphedema exercises like arm raises, shoulder rolls, and arm bends encourage muscles to act like a pump to promote the flow of fluid out of swollen areas.
- Skin care: Skin care for lymphedema is a key component of CDT, as it helps reduce the possibility of infection, which can worsen symptoms. Keeping nails trimmed, wearing sunscreen, and wearing moisturizer are all ways to maintain healthy skin.
How long should I wear my lymphedema sleeve?
Compression arm sleeves play an important role in any upper body lymphedema treatment plan. Most lymphedema arm sleeves can be worn throughout the day and taken off at night unless advised otherwise by your lymphedema specialist.
Pneumatic compression devices can be used to complement arms sleeves for a more targeted approach. These arm pumps for lymphedema must be recommended by a doctor and used once per day with various cycles ranging from 12 to 60 minutes . Pneumatic compression devices differ from compression garments, in that they deliver intermittent pressure to create a “work and release” motion that mimics the techniques of a manual lymphatic drainage to promote the flow of fluid.
What is the difference between the Flexitouch Plus and Nimbl systems?
Tactile Medical’s Flexitouch Plus and Nimbl systems are both pneumatic compression devices that are designed for the self-management of lymphedema symptoms at home. Both lymphedema products have upper body components for those living with lymphedema in areas like the arms.
The Flexitouch Plus system offers more comprehensive treatment with vest and arm garments to cover the entire chest, arm and hand. ComfortEase™ increases treatment coverage and includes a simultaneous bilateral treatment option for greater efficiency.
The Nimbl system is another lymphedema compression pump for the arm, but is designed only for the arm and hand. This simple pneumatic compression pump is often required as a first step by most insurance providers. With eight chambers that inflate sequentially from your fingertips toward your body, the Nimbl system can efficiently move excess fluid from swollen areas.
1. Rockson S. Lymphedema after Breast Cancer Treatment. N Engl J Med. Nov. 15, 2018.
2. Ridner S, McMahon E, Dietrich M, et al. Home-Based Lymphedema Treatment in Patients with Cancer-Related Lymphedema or Noncancer-Related Lymphedema. Onc Nurse Forum. July 2008 Vol. 35(4); 671-680.