Lower Extremity Lymphedema Treatment
Lymphedema is a chronic, progressive condition that’s the result of an impaired lymphatic system, leading to swelling. Discover lower body lymphedema treatment solutions that promote lymphatic circulation in regions like the feet, legs, and lower abdomen.
Find Relief at Home with the Flexitouch® Plus or Nimbl™ systems
Enjoy targeted relief from swelling and related lower extremity lymphedema symptoms with pneumatic compression devices like the Nimbl™ or Flexitouch® Plus system. These lymphedema pumps are designed to be used once an hour each day to encourage the flow of fluid to reduce chronic swelling, helping patients enjoy a better quality of life. Paired with lymphedema garments like compression socks and sleeves that can be worn daily, Nimbl and Flexitouch Plus systems are excellent for symptom management.
Flexitouch Plus provides a comfortable, effective, at-home treatment designed to help head and neck lymphedema patients get back to their lives.
The Flexitouch Plus system moves lymph fluid to reduce swelling. It is clinically proven to stimulate the lymphatic system, enhance quality of life and reduce episodes of cellulitis.
Flexitouch Plus helps patients self-manage their lymphedema, chronic venous insufficiency (CVI) and nonhealing
venous leg ulcers with:
Clinically Proven: Clinical evidence shows that Flexitouch is proven to work better than self-manual lymphatic drainage (MLD), basic pumps or standard therapy with self-care alone.
Consistent: High patient satisfaction encourages ongoing use and better outcomes.
Comfortable: Garments are made of soft, comfortable fabric.
Convenient: Garments are designed for ease of use, and even the ability to treat both legs at the same time.
Discover
Nimbl™
for Lower Body
Innovative and effective basic pneumatic compression therapy for the lower body, with a small, light, compact, and connected controller designed for an improved patient experience.
Discover
Flexitouch® Plus
for Lower Body
Empowering patients to self-manage their lower extremity lymphedema, venous insufficiency and nonhealing venous leg ulcers from home helps improve outcomes and quality of life.4, 5
Lymphedema can be debilitating and can lead to serious skin infections and wounds.
Chronic swelling in the lower body can be a challenge to diagnose because there are many potential causes. If the cause is lymphedema, it can also be difficult to manage because there currently is no “simple fix,” such as a pill to take. In the absence of appropriate treatment, lower extremity lymphedema can cause skin infections, like cellulitis, permanent internal scarring (fibrosis) and other serious skin changes or wounds.
As with any chronic, progressive condition, early intervention and practical tools for daily management create the best results.
Discover Our Solutions
No matter where you may have swelling, we can help.
In many cases, the sooner you treat chronic swelling, the better for your long-term health. Our at-home lymphedema therapy solutions are designed with patient-centered care in mind, focusing on comfort, ease of use, and improved patient outcomes so you can treat your swelling on your own time to help you get back to living your best life.
Upcoming webinars
Register for our upcoming live webinars or take a look at past webinars and other resources for the latest research
Need help now? We’re here for you.
Call us at 1.833.3TACTILE (1-833-382-2845)
Lower Body Lymphedema FAQs
What is lower body lymphedema?
Lymphedema in the lower body, such as the legs, groin, abdomen, or trunk, is a chronic, progressive condition caused by an abnormal accumulation of fluid that results in localized swelling. Lymphedema occurs when the lymphatic system, which includes lymph nodes and vessels, is unable to drain lymph fluid from tissues properly. Lymph nodes act as filters and play a crucial role in maintaining fluid balance and immune function.
What causes lower extremity lymphedema?
Lymphedema in the lower body can be classified as primary lymphedema, where the condition is inherited, present at birth, or spontaneous in nature. However, lower body lymphedema is more commonly caused by a disruption to the lymphatic system, known as secondary lymphedema. Common causes of lymphedema in the lower body include:
- Cancer, cancer surgery, and radiation therapy: These can damage or remove lymph nodes and vessels, disrupting lymphatic circulation and causing fluid to build up in the legs.
- Chronic venous insufficiency (CVI): When leg veins can’t effectively return blood to the heart, increased pressure and fluid leakage can strain the lymphatic system and cause persistent swelling.
- Infections: Infections like cellulitis can inflame and scar lymph vessels, reducing their ability to drain fluid properly. Maintaining healthy circulation in the legs is crucial for reducing the risk of infections and promoting tissue healing in patients with lymphedema.
- Obesity: Excess body fat can compress lymph nodes and lymphatic vessels, making it harder for fluid to circulate, resulting in swelling. Maintaining a healthy weight and managing obesity can help reduce your risk of developing lymphedema.
- Blood clots: Also known as deep vein thrombosis, blood clots can block normal blood and lymph drainage, leading to swelling and long-term lymphatic damage.
- Trauma: Direct trauma from an injury like a crushing accident or burn can damage lymph nodes and vessels, making it difficult to drain and circulate fluid properly
While lymphedema is a chronic and progressive condition, there are ways to manage swelling, pain, and related symptoms, such as lymphedema compression garments, lymphedema pumps that deliver pneumatic compression, exercise, and lifestyle modifications.
What is the difference between lower body and upper body lymphedema?
Extremity lymphedema can affect both the upper and lower limbs and shares the same underlying cause, which is impaired lymphatic drainage. Upper extremity lymphedema often affects the hand, arm, or chest wall, and typically develops after breast cancer treatment or radiation therapy that removes or damages lymph nodes in the underarm.
Lower extremity lymphedema involves the legs, feet, or lower abdomen and is more commonly associated with conditions affecting the legs, such as chronic venous insufficiency, pelvic surgery, obesity, or infections. Because the legs carry more body weight and handle higher fluid pressure, lower extremity lymphedema often leads to more severe swelling, mobility challenges, and skin complications than upper extremity lymphedema.
What are the symptoms of lymphedema in the legs?
Lymphedema is a chronic and progressive condition, which means symptoms may start out mild and progress in severity if treatment and management approaches aren’t taken. Understanding lymphedema risk factors and the symptoms to look out for can help ensure a proper diagnosis and treatment plan. Some of the common symptoms of lymphedema in the legs include:
- Swelling
- Pain, discomfort, and tightness
- Skin changes
- Increased risk of infections
- Decreased range of motion
- Fibrosis
- Pitting edema
- Fatigued, heavy limbs
How do you treat lower body lymphedema?
While the symptoms of lymphedema can progress, such as increased swelling and pain, there are several treatment methods patients can implement to reduce the progression of symptoms. Complete decongestive therapy (CDT) is the standard lymphedema treatment approach, and is a multimodal treatment plan that starts with in-clinic treatment provided by a certified lymphedema therapist, followed by at-home self-management with tools like pneumatic compression devices to reduce swelling. Below are the main components of CDT:
- Manual lymphatic drainage (MLD): MLD is a specialized massage technique that promotes drainage in the lymphatic system by guiding fluid out of the affected area for recirculation. After a lymphedema therapist or doctor gives direction, patients can perform self-manual lymphatic drainage massages at home. Pneumatic compression devices, such as the Nimbl or Flexitouch Plus systems, provide safe and effective MLD for home maintenance. These lymphedema pumps should be worn for an hour each day to aid in the drainage of fluid.
- Compression: Compression bandaging and compression garments for legs are used to promote the flow of fluid to reduce and maintain the reduction of swelling. Compression bandaging applied by a lymphedema therapist is common in Phase I, known as Active CDT, while compression garments for lymphedema, like compression socks, are used in Phase II, known as Maintenance CDT.
- Exercise: Regular exercise can also relieve swelling and related lymphedema symptoms. Performing lymphedema exercises prescribed by a lymphedema therapist, such as walking, yoga, or swimming, activates the muscles, which then act as a pump to promote the flow of fluid back into the bloodstream toward the heart. Maintaining a healthy weight through diet and regular physical activity is an important part of managing lymphedema. Obesity can worsen swelling and make symptoms more difficult to control, so weight management should be a key component of your treatment plan.
- Skin and nail care: Following nail and skin care best practices is another key component of any lymphedema treatment plan. It helps prevent cuts and the risk of infection, which can further exacerbate swelling, pain, and other symptoms. Moisturizing, keeping nails trimmed, and wearing sunscreen help ensure the skin on the affected area is protected.
How do pneumatic compression devices work?
Pneumatic compression devices, such as the Nimbl or Flexitouch Plus system, are some of the best pneumatic compression garments for lymphedema of the legs, as they deliver mild, dynamic pressure in set intervals in a wave-like motion to direct fluid from impaired regions to healthier areas of the body. This gentle “work and release” action stimulates the lymphatics to encourage the flow of fluid to be absorbed and processed by the body. When lymph nodes are unable to filter and move lymph fluid effectively, pneumatic compression devices can help stimulate lymphatic flow and support the body’s natural drainage processes.
Tactile Medical’s Nimbl system is a compact, user-friendly basic pneumatic compression device that has eight compression chambers. Its multiple pressure modes allow for individualized treatment, and the unique inflation sequencing ensures a more comfortable patient experience. Tactile’s Flexitouch Plus system is a pneumatic compression device with lower body compression garments for half-leg treatment, full-leg treatment, or full-leg and core treatment. New ComfortEase garments make it easier for patients to take these garments on and off, as well as fit a wider range of body types. Contact us to learn more about our lymphedema therapy for legs and how they can help you find personalized relief.
What are lymph nodes, and why are they important in lymphedema?
Lymph nodes are small, bean-shaped structures that are part of the lymphatic system. They filter lymph fluid and help fight infection. In the lower body, clusters of lymph nodes in the groin (inguinal lymph nodes) are especially important for draining fluid from the legs and lower abdomen.
Secondary lymphedema often develops after lymph nodes are removed or damaged during cancer surgery or radiation therapy. When lymph nodes are missing or impaired, lymph fluid can accumulate in the lower body, leading to chronic swelling.
What should patients expect when starting at-home lymphedema therapy?
Patients should follow a regular routine that includes compression therapy, gentle exercise, and skin care. A certified lymphedema therapist will prescribe a personalized treatment plan that adheres to the principles of phase II of complete decongestive therapy.
Patients will wear compression garments or bandages, perform manual lymphatic drainage, complete specific, gentle exercises that improve lymph flow, and conduct daily skin care to prevent infections. Once per day, or as recommended by their doctor, patients will also use their pneumatic compression device, such as the Flexitouch Plus or Nimbl, to direct fluid from the affected region to healthier areas of the body to combat chronic swelling.
How do patients know if they are eligible for pneumatic compression devices?
In order to be eligible for a pneumatic compression device (PCD), such as Tactile Medical’s Flexitouch Plus or Nimbl, patients will need a prescription from their doctor. Specific criteria will often need to be met, such as having a documented diagnosis and a failure to get relief from other forms of lymphedema treatment, such as manual lymphatic drainage or compression garments.
Learn how to talk to your doctor about a PCD and explore how to receive health plan reimbursement and insurance coverage. At Tactile Medical, we partner with clinicians and health plans so you can get the at-home treatment needed to manage your lymphedema symptoms.
What support is available for patients using Flexitouch Plus or Nimbl systems?
At Tactile Medical, our Customer Care Team is on standby to offer any support needed for patients using Flexitouch Plus or Nimbl systems. Patients can also use the Kylee App, which is a free mobile app for tracking treatment and learning about lymphedema. We also have dedicated support pages with in-depth information, including our Flexitouch Plus support page and Nimbl support page. Patients can also browse our Resource Hub, which features a range of in-depth articles covering topics related to lymphedema, lipedema, chronic venous insufficiency, and related topics. Contact us today to get the support you need.
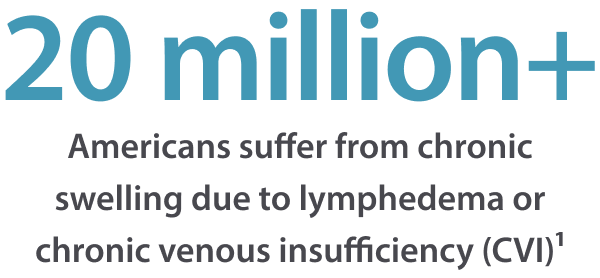
1. Dean S, Valenti E, Hock K, Leffler J, Compston A, Abraham W. The Clinical Characteristics of Lower Extremity Lymphedema in 440 Patients. Jour of Vasc Surg: Venous & Lymph Disorders. ePublished Feb 2020.
Data on file at Tactile Medical
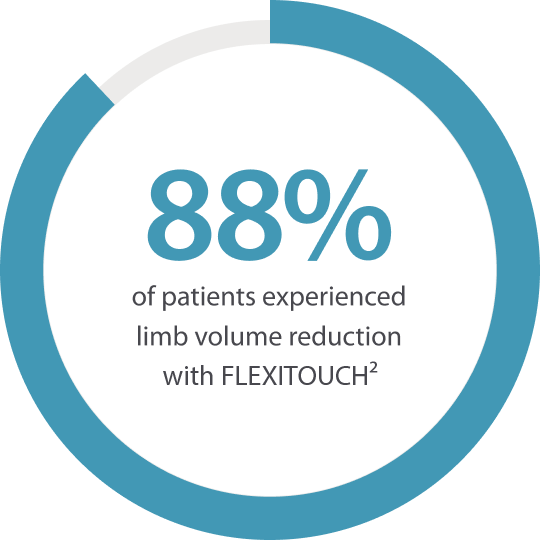
2. Muluk SC, Hirsch AT, Tafe EC. Pneumatic Compression Device Treatment of Lower Extremity Lymphedema Elicits Improved Limb Volume and Patient-reported Outcomes. EJVES. 2013; Vol. 46(4): 480–487.
3. Fife C, Davey S, Maus E, et al. A Randomized Controlled Trial Comparing Two Types of Pneumatic Compression for Breast Cancer Related Lymphedema Treatment in the Home. Supportive Care Cancer. Dec;20(12):3279-86 2012.
4. Muluk SC, Hirsch AT, Tafe EC. Pneumatic Compression Device Treatment of Lower Extremity Lymphedema Elicits Improved Limb Volume and Patient-reported Outcomes. EJVES. 2013; Vol. 46(4): 480–487.
5. Adams, KE, Rasmussen JC, Darne C, et al. Direct Evidence of Lymphatic Function Improvement After Advanced Pneumatic Compression Device Treatment of Lymphedema. Biomedical Optics Express. 2010; Vol. 1(1): 114–125.
6. Karaca-Mandic P, Hirsch AT, Rockson SG, et al. The Cutaneous, Net Clinical, and Health Economic Benefits of Advanced Pneumatic Compression Devices in Patients With Lymphedema. JAMA Dermatol. 2015;151(11):1187–1193.
7. Muluk SC, Hirsch AT, Tafe EC. Pneumatic Compression Device Treatment of Lower Extremity Lymphedema Elicits Improved Limb Volume and Patient-Reported Outcomes. EJVES. 2013; Vol. 46(4): 480–487.
8. Adams, KE, Rasmussen JC, Darne C, et al. Direct Evidence of Lymphatic Function Improvement After Advanced Pneumatic Compression Device Treatment of Lymphedema. Biomedical Optics Express. 2010; Vol. 1(1): 114–125.
9. Blumberg S, Berland T, Rockman C, Mussa F, Brooks A, Cayne N, Maldonado T. Flexitouch – Pneumatic Compression Improves Quality of Life in Patients with Lower-Extremity Lymphedema. Annals of Vascular Surgery. 2015; Vol. 29(4): 628-629.
10. Ridner S., McMahon E., et al. Home Based Lymphedema Treatment in Patients With and Without Cancer-Related Lymphedema. Oncology Nursing Forum. 2008; Vol. 35(4): 671–680.
11. Lerman M, Gaebler J, Hoy S, Izhakoff J, Gullett L, Niecko T, Karaca-Mandic P, O’Donnel T, Rockson S. Flexitouch Advanced Pneumatic Compression Device Reduces Phlebolymphedema Healthcare Costs Compared to Other Treatment Modalities. Journal of Vascular Surgery. June 2018.
12. Fife C, Davey S, Maus E, Guilliod R, Mayrovitz H. A Randomized Controlled Trial Comparing Two Types of Pneumatic Compression for Breast Cancer Related Lymphedema Treatment in the Home. Supportive Care in Cancer 2012.