Lymphedema and Weight Loss
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More
Stage three lymphedema is the most advanced stage of this chronic condition. In this stage, the affected body part might display one or more symptoms, such as significant swelling, alterations in the skin, or recurring episodes of infection. While this stage can be challenging to manage, understanding your condition and working with healthcare professionals can help you maintain your quality of life and prevent complications.
Let’s explore what you need to know about managing stage 3 lymphedema and the treatment options available.
The third stage of lymphedema is the most advanced phase of this progressive condition of the lymphatic system. At this stage, the affected body part can experience severe, chronic swelling, leading to permanent changes in the tissue and skin. However, not every patient with stage 3 lymphedema will experience limb overgrowth and/or disfiguration, which can make it difficult for doctors to diagnose. This means stage 3 lymphedema can also be defined by tissue changes and fibrosis, infection, and ulceration, and may or may not occur with a largely edematous limb.
Unlike earlier stages, stage 3 lymphedema is characterized by hardened tissue and significant changes in the size and shape of the affected area.1
This advanced stage differs from earlier phases of lymphedema. Stage 1 is generally characterized by mild swelling that subsides with elevation and is reversible, whereas stage 2 exhibits more consistent swelling along with some tissue alterations. In stage 3, however, irreversible and significant changes occur with progressive swelling, skin changes and infection.2
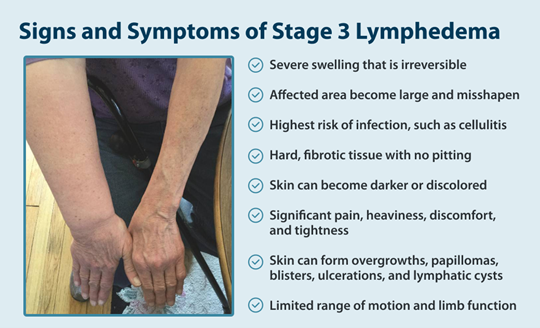
Understanding the signs of lymphedema at this advanced stage ensures proper management and care. The symptoms of stage 3 lymphedema are more severe and noticeable than in earlier stages and may include one or several of the following symptoms in combination:
Understanding the causes of lymphedema can help explain how the condition progresses to stage 3. Two main types of lymphedema exist: primary and secondary lymphedema.
Primary lymphedema is a result of genetic factors that result in malformation of the lymphatics during the systems development in the embryo. This results in either too few, too many or simply dysfunctional lymphatic vessels that cannot properly drain fluid from the tissues. The effects can be present at birth or develop later in life. If not properly managed, people born with primary lymphedema can progress to having more severe lymphedema over time.
Secondary lymphedema is more common and develops after direct trauma or damage to the lymphatic system. This damage can result from a number of causes, but typically include cancer and its treatment, chronic venous insufficiency, trauma, obesity, or infection. Understanding lymphedema risk factors is crucial, as early intervention can help prevent progression to stage 3.3
Accurate diagnosis ensures proper treatment planning and management of stage 3 lymphedema. Healthcare providers use several methods to confirm the condition and rule out other conditions:
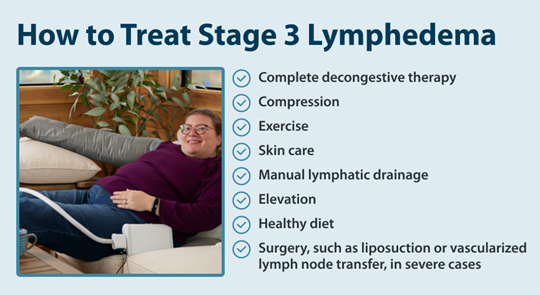
Learning how to treat lymphedema is crucial once you reach stage 3. While earlier intervention is ideal, implementing a comprehensive treatment plan at any stage can help manage symptoms and prevent complications. A combination of various therapeutic approaches can help control swelling, maintain skin health, and improve your quality of life. Here’s a detailed look at each treatment method:4
While living with stage 3 lymphedema comes with unique challenges, maintaining a consistent treatment routine can help you manage symptoms effectively and prevent complications.
For many people with lymphedema, at-home treatment options can complement professional care. Tactile Medical’s lymphedema products, including the Flexitouch Plus and Nimbl systems, are doctor-prescribed pneumatic compression devices that you can use in the comfort of your own home. These systems provide consistent, effective compression therapy to help manage symptoms. Remember, while stage 3 lymphedema is a chronic condition, you can continue to live an active and fulfilling life with proper care and support.
References:
1. “NCI Dictionary of Cancer Terms.” Comprehensive Cancer Information – NCI, www.cancer.gov/publications/dictionaries/cancer-terms/def/stage-iii-lymphedema.
2. “Lymphedema Stages.” Breastcancer.Org – Breast Cancer Information and Support, Breastcancer.org, 15 Aug. 2023, www.breastcancer.org/treatment-side-effects/lymphedema/stages.
3. “Ask the Doctors: Lymphedema Symptoms and Causes with Doctors Sacks and Anolik.” Department of Surgery, 3 July 2023, surgery.wustl.edu/ask-the-doctors-lymphedema-symptoms-and-causes/.
4. “Treating Lymphedema.” Johns Hopkins Medicine, 1 Aug. 2024, www.hopkinsmedicine.org/health/treatment-tests-and-therapies/treating-lymphedema
5. Park, Kitae E, et al. “Surgical Management of Lymphedema: A Review of Current Literature.” Gland Surgery, U.S. National Library of Medicine, Apr. 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7225501/.
Living with lymphedema while trying to manage your weight can feel overwhelming, but understanding the connection between lymphedema and weight loss can help you develop effective strategies for both conditions.
Read More
When the lymphatic system becomes compromised, fluid buildup can lead to stage 1 lymphedema, a condition marked by mild but noticeable swelling in affected areas. This initial stage is a crucial window for intervention, as proper treatment can prevent progression to more severe stages. Knowing the signs, causes, and treatment...
Read More
Living with stage 2 lymphedema brings unique challenges, but understanding your condition is the first step toward effectively managing it. While this stage marks a point where the condition becomes irreversible, there are many ways to maintain your quality of life and prevent symptoms from progressing. Keep reading to explore...
Read More
Read More
Call us at 1.800.575.1900