Is Lymphedema Genetic
Hereditary Lymphedema: Is Lymphedema Genetic?
Living with lymphedema can make several aspects of your life more challenging. With that said, you may have several questions. Is lymphedema genetic, and do you have to worry about passing it to your kids? If you have a parent with lymphedema, does that mean you’re more at risk of developing lymphedema yourself? In this guide, we’ll talk about whether or not lymphedema is genetic and break down the different types of lymphedema. If you want to learn more about what causes lymphedema and whether hereditary lymphedema exists, keep reading.
What Is Lymphedema?
Is Lymphedema Genetic?
Primary vs. Secondary Lymphedema
What Are the Types of Primary Lymphedema?
Are There Treatments for Genetic Lymphedema?
Other Causes of Lymphedema
Wrapping Up: Genetic Lymphedema
What Is Lymphedema?
Lymphedema is a medical condition characterized by a build up of excess fluid in the tissues. Your lymphatic system is responsible for several functions, including maintenance of fluid balance, absorption of dietary fats from the digestive system, and immunity to help fight infection. Typically, fluid travels through lymph vessels and lymph nodes and is returned to the bloodstream. In lymphedema patients, a blockage can form in the lymphatic system, preventing fluid from returning to the bloodstream. This blockage can cause swelling due to fluid building up in your lymphatic system and tissue.
Swelling that lymphedema patients experience can lead to numerous symptoms, including a tight feeling in the skin, pain, and decreased mobility. These symptoms can impact your quality of life, which is why it’s so important to talk to your doctor about managing lymphedema after you’ve been diagnosed. The sooner you get on a lymphedema treatment and management plan, the better you can manage your symptoms and prevent their progression.
Is Lymphedema Genetic?
Like many medical conditions, some people are at higher risk of developing lymphedema. So, is lymphedema genetic?
While lymphedema is often caused by surgery or direct trauma or injury to the lymphatic system, that’s not always the case. While more rare, lymphedema can also be a result of a genetic mutation, either hereditary or spontaneous, which is known as primary lymphedema. Primary lymphedema is a result of a genetic mutation during embryological development, and some people experience the signs of lymphedema at a very young age. There are also different types of primary lymphedema, which vary in terms of the time of onset and the exact cause of the condition.
Primary vs. Secondary Lymphedema
An individual can develop two types of lymphedema: primary lymphedema and secondary lymphedema.
Primary lymphedema is due to a genetic malformation of the lymphatic system during embryological development. It can either happen spontaneously in nature, or be due to a hereditary condition, where the gene mutation was inherited or passed down from a parent. Either way, it results in the lymphatic vessels and lymph nodes not being properly formed with impaired function. Different forms of primary lymphedema occur, with a variety of symptoms, and are typically classified by age of onset.
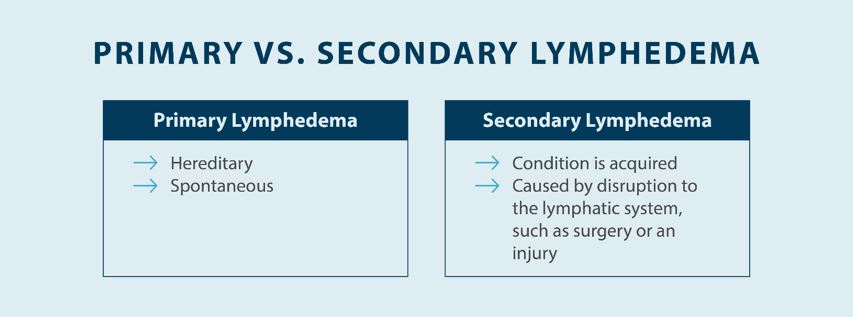
Secondary lymphedema is any type of lymphedema that’s not related to genetics. There are several potential causes of secondary lymphedema, including but not limited to cancer, surgery involving the lymphatic system, and direct injury or trauma to the lymphatics. When any part of your lymphatic system is damaged and unable to function properly, it can lead to the accumulation of lymph in your tissue. This is common in cancer patients who have lymph nodes removed or undergoes radiation therapy, which can damage intact lymph vessels and nodes.
What Are the Types of Primary Lymphedema?
As previously mentioned, there are different types of primary lymphedema. In some cases, primary lymphedema is present at a very early age and inherited or passed down from parent to offspring, known as hereditary lymphedema, which is rare. More often, primary lymphedema begins during adolescence, known as spontaneous lymphedema where an isolated event in nature causes the condition, as opposed to secondary lymphedema, which will occur at the time of injury or insult to the lymphatic system. Below, we’ll provide a breakdown of the different types of hereditary lymphedema and what differentiates each type.
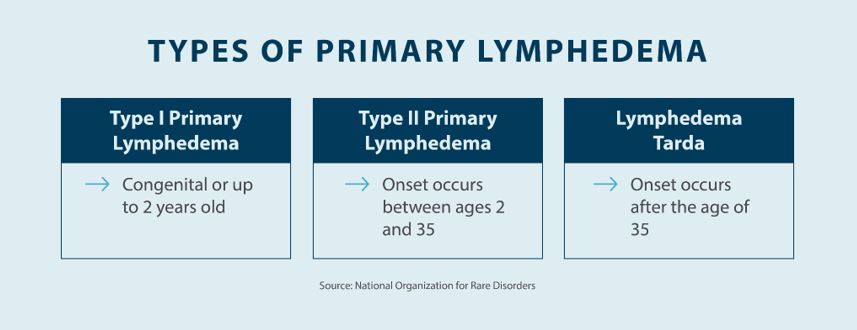
Type I Primary Lymphedema
Type I primary lymphedema is also known as Milroy disease, which is often caused by mutations in the FLT4 gene.1 Because this gene is partially responsible for the development of the lymphatic system, people with type I primary lymphedema typically experience symptoms at a very early age. In most cases, type I primary lymphedema occurs between birth and two years old.1
In some cases, ultrasound scans can determine whether or not a fetus in the womb is affected by type I primary lymphedema. Affected fetuses typically experience swelling in the feet during the second or third trimester of pregnancy, so routine ultrasounds can be an essential part of early diagnosis and treatment of primary lymphedema.
Type I primary lymphedema can vary in terms of the severity of the swelling and where that swelling is located. Swelling in the legs and feet is most common, and it’s rare for that swelling to occur later on in life. However, some patients may experience swelling in other parts of the body, including the genitals. Other complications may arise with type I primary lymphedema, including hydroceles, wart-like growths, and problems with the growth of the toenails.1
For people with type I primary lymphedema, early treatment is key. A lymphedema treatment and management plan can help you control the symptoms of lymphedema at an early age, which can help increase your quality of life and prevent the progression of lymphedema complications.
Type II Primary Lymphedema
Type II primary lymphedema is known as Meige disease or lymphedema praecox.1 While there’s no exact known cause of type II primary lymphedema, it’s generally thought to be a genetic condition because it’s present in patients who haven’t had surgery or trauma involving the lymphatic system.
Type II primary lymphedema varies from type I because it typically affects individuals during the adolescent stage. While Meige disease can also affect people who are younger or older, it generally occurs around the age of puberty. Some people develop type II primary lymphedema shortly after puberty. In addition to occurring at a slightly later age than type I primary lymphedema, type II is the most common type of genetic lymphedema.1
Like other types of lymphedema, type II primary lymphedema very commonly affects the legs. However, people with type II primary lymphedema may also experience swelling in other parts of the body, including the arms, face, and neck area. While swelling that results from lymphedema doesn’t always cause pain, some people with lymphedema can experience pain and discomfort.
Because of the age group that type II primary lymphedema commonly affects, treatment is essential when it comes to managing symptoms. While there is no way to prevent lymphedema and stop swelling and other symptoms, managing lymphedema can help make life easier and prevent complications that may arise in severe cases.
Lymphedema Tarda
The third type of primary lymphedema is known as lymphedema tarda. Unlike other types of primary lymphedema, lymphedema tarda occurs later in life. In fact, lymphedema occurs clinically after the age of 35.2
Lymphedema tarda most commonly affects the legs and lower body, like other types of lymphedema, but it may affect other areas, such as the arms or abdomen. As far as symptoms go, the swelling that lymphedema tarda causes may or may not result in pain and discomfort. While some patients feel pain, many patients spot visible swelling as the first recognizable symptom of lymphedema tarda.
The good news is that lymphedema tarda is a rare form of lymphedema, much like Milroy’s disease. This type of lymphedema only accounts for a small percentage of all cases of primary lymphedema, so genetic forms of lymphedema are more common in adolescents. That being said, it’s a good idea to monitor the signs of lymphedema throughout your life because early treatment and management can help prevent the progression of this condition.
In most cases, treatment for lymphedema tarda is focused on minimizing symptoms and preventing its progression. Treatment options, such as compression garments and devices, can help relieve some of your swelling and reduce your symptoms.
Are There Treatments for Genetic Lymphedema?
Generally speaking, there’s no cure for any type of lymphedema. If your lymphatic system is damaged or hasn’t fully developed, there is no solution to cure this condition. Instead of focusing on a cure, lymphedema treatment focuses on providing relief from symptoms to improve your quality of life and prevent the progression of these symptoms.
Complete decongestive therapy (CDT) is a common treatment option for lymphedema patients. CDT combines several treatment options, including compression, skin care, exercise, and manual lymphatic drainage. Manual lymphatic drainage involves stimulating various parts of the lymphatic system to help encourage drainage through a gentle massage. Lymphatic drainage massages can be performed at home, and your lymphedema specialist or therapist can demonstrate the proper techniques so you can get relief from your symptoms at home.
Compression therapy is one of the best treatment options for patients with lymphedema, whether it’s primary or secondary. Compression garments and devices apply gentle pressure to areas where swelling occurs, which helps guide the flow of fluid away from swollen parts of the body. There are different types of devices that can treat swelling in your arms, legs, and even your head and neck.
Examples include compression stockings, compression bandages, and pneumatic compression devices, such as Tactile Medical’s Flexitouch Plus System. The Flexitouch Plus System provides upper body, lower body, and head and neck lymphedema treatment through gentle compress and release actions. With the ability to find relief from the comfort of your home, you can regain your standard of living.
Exercise is another crucial component of treating and managing lymphedema. Obesity and a lack of exercise are two contributing factors to lymphedema, and exercise can help you maintain a healthy weight. Staying active also helps encourage the flow of lymph throughout your body, which can help relieve swelling and discomfort.
Other Causes of Lymphedema
Knowing the potential causes of lymphedema is vital when understanding how to prevent lymphedema. Anyone can get lymphedema as a result of trauma to the lymphatic system, but there are also some risk factors that you can avoid to lower your risk. Here are some of the non-hereditary causes of lymphedema:

- Cancer surgery: Cancer patients undergoing surgery to remove a lymph node often experience lymphedema. Lymphedema can also occur after a biopsy to test for cancer in the lymph nodes. Essentially, any type of surgery that involves the lymph nodes or lymphatic system can lead to lymphedema.
- Radiation therapy: Radiation therapy can cause damage to the lymphatic system that can lead to a blockage. Scarring may cause a blockage in the lymphatic system in areas where cancer patients have undergone radiation therapy.
- Acute injuries: Acute injuries to the lymphatic system can damage nodes and vessels, such as an injury from a car accident or a sporting accident, which can also lead to lymphedema.
- Vascular diseases: Certain vascular diseases, such as chronic venous insufficiency or blood clots, may increase your risk of developing lymphedema, so it’s important to talk to your doctor about any medical conditions you may have.
- Obesity: People who are overweight are more likely to develop lymphedema, so diet and regular exercise can help you improve the function of your lymphatic system while preventing lymphedema and other potential health problems.
Wrapping Up: Primary Lymphedema
So, is lymphedema genetic? Depending on your medical history and when you developed your lymphedema, it may be. Understanding the cause of your lymphedema can help you determine the best treatment and management plan for your situation, although compression therapy and exercise are typically the recommended treatment options.
If you’re looking for relief from primary or secondary lymphedema, Tactile Medical can help. Our Flexitouch Plus System provides the gentle compression you need to encourage the flow of fluid, reducing swelling and helping to prevent primary and secondary lymphedema complications. This compression device is available for your legs, arms, and even your head and neck. If you need relief from lymphedema, try the Flexitouch Plus System from Tactile Medical today.
Sources:
1. Anguiano, Beatriz, et al. Hereditary Lymphedema. National Organization for Rare Disorders. Accessed August 25, 2022. https://rarediseases.org/rare-diseases/hereditary-lymphedema/
2. Nitti, Matthew, et al. Definition, Incidence and Pathophysiology of Lymphedema. Principles and Practice of Lymphedema Surgery. Accessed August 25, 2022. https://www.sciencedirect.com/topics/medicine-and-dentistry/lymphedema-tarda