Peripheral Edema
Review our guide on peripheral edema to learn about its symptoms, causes, and treatment, so you can manage your condition.
Read More
Cellulitis is a bacterial skin infection that can occur anywhere on the body. Left untreated, cellulitis can lead to further health complications, which is why finding treatment early on is essential. Cellulitis can be caused by a wide range of factors, such as cuts and wounds from surgery. If you’re at risk of developing cellulitis, it’s important to be informed of the causes, symptoms, and treatment of this infection. In this post, we’ll provide an in-depth cellulitis definition, along with information on cellulitis symptoms, what causes cellulitis, treatment options, and more.
What is a cellulitis infection? Cellulitis is a bacterial infection that affects deeper layers of skin. In most cases, cellulitis affects the arms and legs. However, cellulitis can be present anywhere on the body or face, including the abdomen, eyes, anus, and mouth. Cellulitis is transmitted when there is a cut or break in the skin, allowing the bacteria to enter. When a person is infected with cellulitis, they can experience pain and redness in the affected area. Cellulitis is a common bacterial infection, with roughly 14 million Americans being diagnosed with the condition annually.1
Cellulitis is a common skin infection that can lead to further health conditions and even mortality if left untreated. With that said, knowing the signs and symptoms of cellulitis can help you get the proper diagnosis and treatment as soon as possible. In most cases, a person with a lighter complexion will experience redness or pinkness on the area infected with cellulitis. However, on darker skin tones, the infected area may appear gray, dark brown, or purple.
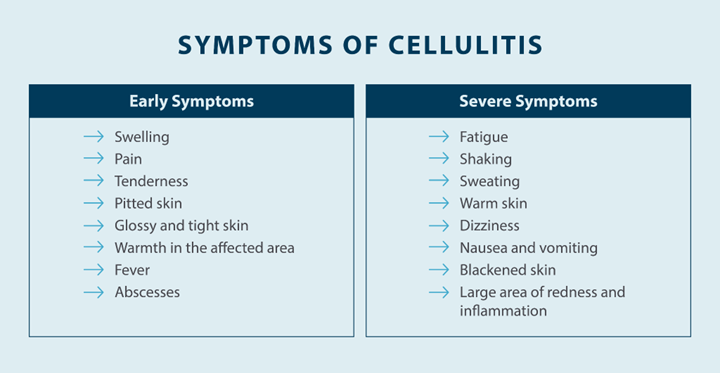
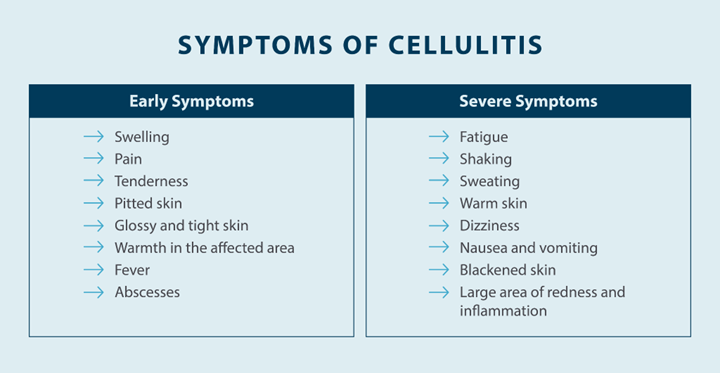
In addition to skin discoloration, there are several common symptoms a patient with cellulitis may experience. However, it’s important to note that symptoms vary from person to person, so they might not appear in each case. Explore common symptoms of cellulitis below:
The above symptoms are often present at the onset of cellulitis. However, if cellulitis goes untreated, more severe symptoms can arise, such as:
No matter the severity of your symptoms, it’s important to seek medical attention right away. However, if you’re experiencing more severe symptoms of cellulitis, such as shaking or dizziness, it can be an indication of a more serious health complication, which will require immediate medical help.
Knowing what causes cellulitis can help prevent the infection from occurring. There are a few different types of bacteria that enter a break in the skin and cause cellulitis. The most common bacteria that cause cellulitis, according to Hopkins Medicine,2 include:
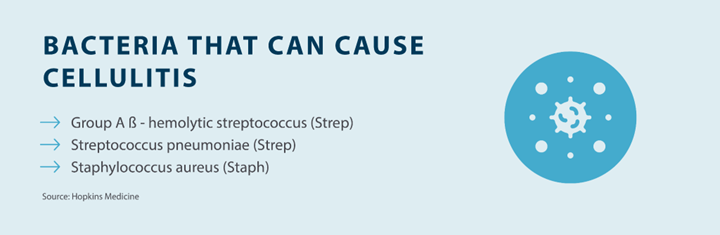
Most staph and strep bacteria are found inside the nose and mouth of people, along with on the skin’s surface, where it is harmless. However, when there is a break in the skin and this bacteria enters, a cellulitis infection can occur.
Some people may be more at risk of being infected with cellulitis than others. Knowing if you’re in an at-risk category can help you get the proper diagnosis and treatment sooner. Below are some risk factors for cellulitis:

There are multiple factors that can put you at risk of being infected with cellulitis. The most common risk factors are any breaks or trauma to the skin that can allow bacteria to enter the deeper layers and cause infection. However, those with a weakened immune system are also at a higher risk of cellulitis, as their bodies have limited protection against the infection.
If you have a weakened immune system or notice any breaks in the skin along with the symptoms of cellulitis, contact your doctor immediately. The sooner you identify cellulitis, the sooner you can get the proper treatment.
As stated, getting treated for cellulitis as soon as you notice symptoms is important. This is because cellulitis can result in several health complications that can be debilitating and even fatal. While complications are uncommon, it’s important to understand what’s at risk if you fail to seek treatment, as the infection can travel to other areas of your body, such as your blood, bones, and muscles. Below are a few complications of cellulitis1,3:
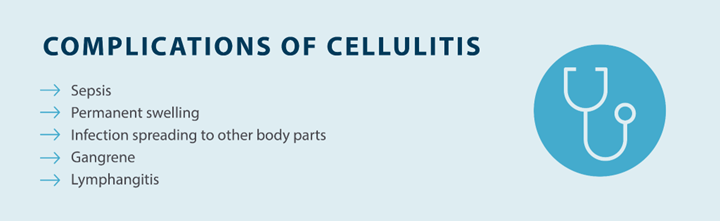
These are some of the complications that can arise if cellulitis goes untreated, which is why it’s important to seek medication attention at the onset of any symptoms.
Cellulitis can be painful and uncomfortable. Finding ways to prevent cellulitis is essential to ensuring your health and safety. Whether you’re in an at-risk category or you have a recent break in your skin, follow these measures to help prevent cellulitis:
An important step to preventing cellulitis is to take proper care of any cut or wound to prevent bacteria from entering the body. This is especially true if you have poor circulation or any underlying health conditions that can put you at greater risk of cellulitis.
No, in most cases, cellulitis is not contagious. Cellulitis isn’t an airborne disease, which means it can’t be spread if someone infected with cellulitis is breathing close to you. However, cellulitis can be spread if you have an open cut or wound that comes into contact with skin with an active cellulitis infection.
If you have a cut or open wound that begins to swell, turn red, feel warm, or become painful, you should visit your doctor right away. These signs can indicate that you have an infection, such as cellulitis, and the earlier you treat your infection, the sooner you can heal and prevent more serious health complications.
Yes, cellulitis can be treated. The most common form of treatment for cellulitis is antibiotics, which will be prescribed by a doctor after a proper diagnosis. To diagnose cellulitis, a doctor will conduct a physical exam to look for signs of swelling, redness, and warmth and ask about your medical history and any events that could lead to cellulitis, such as a dog bite, wound, or underlying health condition such as lymphedema.
Once diagnosed with cellulitis, your doctor will likely prescribe antibiotics, which are taken orally. However, for more serious infections, intravenous (IV) antibiotics will have to be administered directly into the vein. In most cases, cellulitis will be cured after ten days of taking antibiotics.
In addition to antibiotics, there are a few at-home treatment options that can help patients manage their symptoms, such as:
It’s important to note that these at-home remedies are designed to improve your overall comfort, and antibiotics prescribed by a doctor are the primary source of treatment.
At Tactile Medical, our mission is to improve the lives of people living with lymphedema. Lymphedema is a progressive disease that results in the accumulation of fluid in a localized region of the body, typically the arms or legs. However, it can occur anywhere in the body, such as the head and neck, abdomen, and genital regions. Because lymphedema results in swelling in the affection region, it can cause the skin to crack, making people living with lymphedema more susceptible to cellulitis.
Tactile Medical’s Flexitouch Plus system moves lymph fluid to reduce swelling and in turn, enhance the quality of life and reduce occurrences of cellulitis in patients. In fact, studies found the Flexitouch Plus system to reduce episodes of cellulitis by 81% in patients.4 In addition to reducing episodes of cellulitis in lymphedema patients, the Flexitouch Plus system is clinically proven to work better than self-manual lymphatic drainage (MLD), basic pumps, or standard therapy with self-care alone. With head and neck, upper body, and lower body systems, you can manage your lymphedema from the comfort of your home and reduce symptoms, including cellulitis.
If you’re living with lymphedema, you can be at a heightened risk of cellulitis due to increased swelling that can cause your skin to crack. With Tactile Medical’s Flexitouch Plus system, you can manage your lymphedema at home to reduce swelling and episodes of cellulitis.
References
1. Brown BD, Hood Watson KL. Cellulitis. StatPearls. Accessed March 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK549770/
2. John Hopkins Medicine. Cellulitis. Hopkinsmedicine.org. Accessed March 30, 2022. https://www.hopkinsmedicine.org/health/conditions-and-diseases/cellulitis
3. MedlinePlus. Cellulitis. MedlinePlus.gov. Reviewed April 14, 2021. Accessed March 30, 2022. https://medlineplus.gov/ency/article/000855.htm
4. Blumberg SN et al. Pneumatic Compression Improves Quality of Life in Patients with Lower-Extremity Lymphedema. Annals of Vascular Surgery. May, 2015 Vol. 29(4):628–629. Accessed March 30, 2022. https://tactilemedical.com/wp-content/uploads/2015/05/Clinical-Highlights-FT-Improves-Quality-of-Life-Reduces-Cellulitis-500266-004D.pdf
Review our guide on peripheral edema to learn about its symptoms, causes, and treatment, so you can manage your condition.
Read More
Review our guide on the differences between inflammation vs. swelling, so you can understand how they impact your body differently.
Read More
Review our guide on chronic venous insufficiency (CVI) to better understand the symptoms, causes, and treatment options to get the care you need.
Read More
Read More
Call us at 1.800.575.1900