Overcoming Payer Denials
Denied therapy by your insurance?
Here’s what you can do.
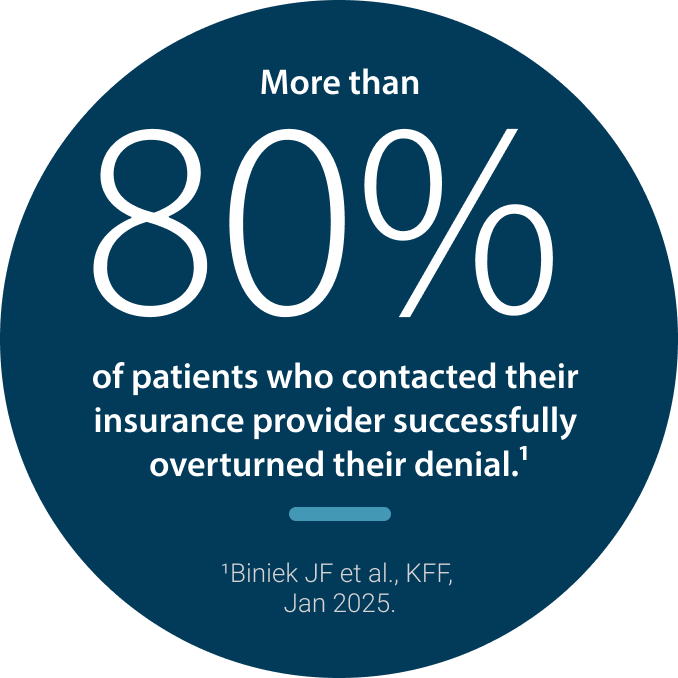
Oftentimes a denial just means the insurance provider needs more information. Statistics show >80% of patients who contacted their health insurance provider successfully overturned their denial.1 That’s why it’s important to know how to work with them to receive the therapy you or a loved one has been prescribed.
This Patient Advocacy Toolkit is designed to help you do this. Download the forms here or learn more about the process below.

Patient Advocacy Toolkit
These resources will help you become your most effective advocate as you reach out to your insurance provider:
1. UNDERSTAND THE APPEAL PROCESS
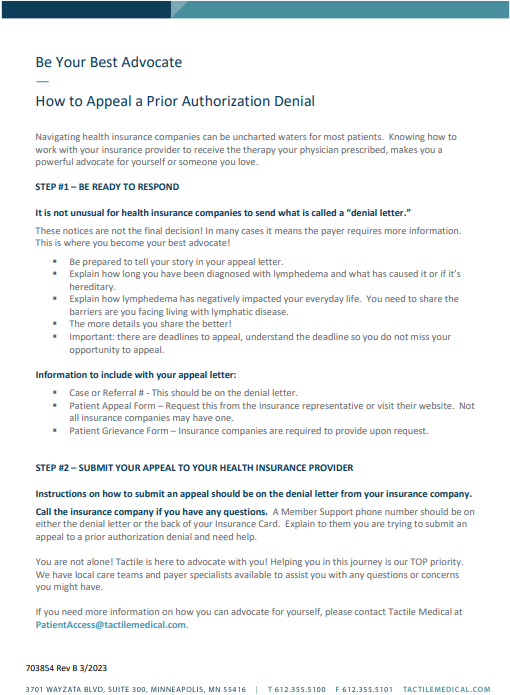
Start by reviewing the overall appeal process. This helps you know what to expect, what your insurance provider requires, and how to track each part of the process. Taking a moment to get grounded makes the next steps easier and more effective.
To get started, download our appeal process document for a clear, step by step overview you can follow.
2. SUBMIT AN ADVOCACY LETTER

When your claim is denied, your first formal response should be a written appeal. Use the sample advocacy letter to explain why the denied service is necessary, provide supporting information, and request that the decision be reconsidered. A clear, organized letter sent by mail or email helps ensure your concerns are documented.
To begin drafting your appeal, download our sample advocacy letter and personalize it to your situation.
3. CALL YOUR INSURANCE PROVIDER

After submitting your letter, follow up with a call to your insurance provider. Use the sample call script to guide the conversation, ask clarifying questions, confirm that your appeal has been received, and document the details of the call. Speaking directly with a representative can help move your appeal forward.
Before you call, download our sample call script so you can follow along with confidence.
From Denial to Approval Through Relentless Advocacy
When their claim was denied, this couple felt frustrated and unsure where to turn. Instead of accepting the decision, they contacted their insurance team, shared their situation, and followed the guidance they were given. Clear communication and persistent follow up helped overturn the denial and secure the coverage they needed.
Watch the full story here →
The Data Is Clear: Appeals Work.
New data shows Medicare Advantage insurers denied more than three million prior authorization requests in 2023, yet more than 80 percent of appealed denials were overturned. The takeaway is simple: when patients push back, coverage often gets approved.
You deserve the therapy your doctor has prescribed and these resources may help you get it. For more advocacy information and support, contact us at